Clinical videos + HTML notes for NEET PG-ready revision.
Streamora lets you upload case-based videos, attach rich HTML notes, like and comment on other clinicians’ posts, follow creators and save structured exam-oriented pearls – all mobile-first and SEO-ready.
Why Streamora stands out for NEET PG aspirants: Unlike generic apps, we focus on high-yield topics like labour stages (from first to fourth, with management pitfalls), Rh-negative pregnancies (anti-D prophylaxis timing), and anatomy pearls (e.g., sacral hiatus for caudal blocks). Our community-driven notes include real residency cases—e.g., "Missed Rh isoimmunization leading to hydrops fetalis"—with attached flowcharts and MCQ-style tags for quick revision. Free, ad-light, and built by med students for med students.
Latest Medical Posts
High-yield medical discussions, NEET PG-flavoured notes and short clinical cases from all users.
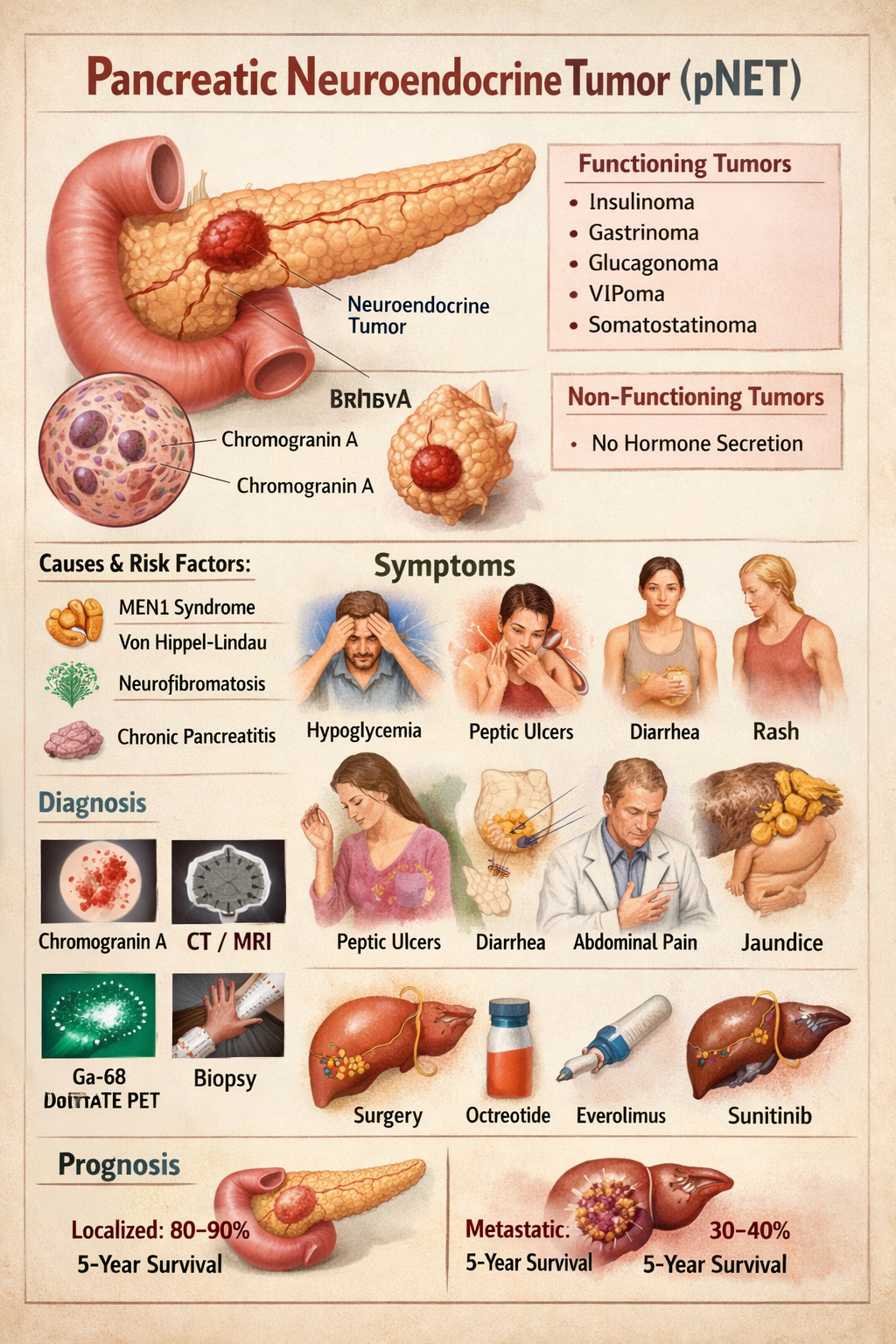
Pancreatic Neuroendocrine Tumor Symptoms Diagnosis Treatment Prognosis
--- # **PANCREATIC NEUROENDOCRINE TUMOR (pNET)** --- ## **1. Definition** Pancreatic neuroendocrine tumors (pNETs) are **neoplasms arising from endocrine (islet) cells of the pancreas** that secrete peptide hormones or amines. They are biologically distinct from pancreatic adenocarcinoma and may be **functioning (hormone-secreting)** or **non-functioning**. --- ## **2. Pathophysiology** pNETs originate from **enterochromaffin cells** of pancreatic islets. They show: * **Neuroendocrine differentiation** * **Dense-core secretory granules** * **Expression of chromogranin A and synaptophysin** Tumor behavior depends on: * **Hormone secretion** * **Tumor size** * **Ki-67 index (mitotic rate)** * **Invasion and metastasis** Tumors may be: * **Well differentiated (NET G1–G3)** * **Poorly differentiated (Neuroendocrine carcinoma)** MEN1 mutation commonly involved → parathyroid, pituitary, pancreas tumors. --- ## **3. Classification** ### **A. By hormone secretion** | Type | Hormone | | --------------- | ------------ | | Insulinoma | Insulin | | Gastrinoma | Gastrin | | Glucagonoma | Glucagon | | VIPoma | VIP | | Somatostatinoma | Somatostatin | | Non-functioning | None | ### **B. By WHO grading** | Grade | Ki-67 | | ----- | ----- | | G1 | <3% | | G2 | 3–20% | | G3 | >20% | --- ## **4. Causes and Risk Factors** * MEN-1 syndrome * Von Hippel–Lindau * Neurofibromatosis-1 * Tuberous sclerosis * Smoking * Chronic pancreatitis --- ## **5. Clinical Features** ### **A. Insulinoma** * Hypoglycemia * Sweating * Palpitations * Confusion * Weight gain ### **B. Gastrinoma (Zollinger-Ellison)** * Severe recurrent peptic ulcers * Diarrhea * GERD ### **C. Glucagonoma** * Diabetes * Necrolytic migratory erythema * Weight loss * Anemia ### **D. VIPoma** * Profuse watery diarrhea * Hypokalemia * Achlorhydria ### **E. Somatostatinoma** * Diabetes * Gallstones * Steatorrhea ### **F. Non-functioning** * Abdominal pain * Weight loss * Jaundice * Abdominal mass * Metastasis symptoms --- ## **6. Investigations** ### **Blood Tests** | Test | Use | | ------------------ | --------------- | | Chromogranin-A | Tumor marker | | Insulin, C-peptide | Insulinoma | | Gastrin | Gastrinoma | | Glucagon | Glucagonoma | | VIP | VIPoma | | Somatostatin | Somatostatinoma | | Fasting glucose | Hypoglycemia | ### **Imaging** * Contrast CT * MRI pancreas * Endoscopic ultrasound (best for small tumors) * Ga-68 DOTATATE PET-CT (gold standard) * Octreoscan ### **Biopsy** * EUS-guided biopsy * Ki-67 index --- ## **7. Differential Diagnosis** * Pancreatic adenocarcinoma * Islet cell hyperplasia * Metastatic carcinoid * Chronic pancreatitis * Insulin autoimmune syndrome --- ## **8. Management** ### **A. Curative – Surgery** * Enucleation (small insulinomas) * Distal pancreatectomy * Whipple procedure * Liver metastasis resection ### **B. Medical Therapy** Used when metastatic, unresectable or hormone excess. --- ## **9. Drugs Used** ### **1. Octreotide** **Indication:** Hormone control and tumor stabilization **Mechanism:** Somatostatin analog → inhibits hormone secretion **Dose:** Adult: 100–500 mcg SC 2–3 times/day or 20–30 mg IM monthly Paediatric: 1–10 mcg/kg/day **Adverse effects:** Gallstones, diarrhea, hyperglycemia **Contraindication:** Severe gallbladder disease **Monitoring:** LFT, glucose **Counsel:** May cause GI upset --- ### **2. Lanreotide** Same as octreotide Dose: 120 mg SC every 4 weeks --- ### **3. Everolimus** **Indication:** Advanced pNET **Mechanism:** mTOR inhibitor **Dose:** 10 mg daily **Adverse:** Mouth ulcers, hyperglycemia, infections **Contra:** Active infection **Monitor:** CBC, glucose **Counsel:** Avoid live vaccines --- ### **4. Sunitinib** **Indication:** Metastatic pNET **Mechanism:** VEGF receptor inhibitor **Dose:** 37.5 mg daily **Adverse:** Hypertension, fatigue **Contra:** Cardiac failure **Monitor:** BP, ECG --- ### **5. Diazoxide (for insulinoma)** **Mechanism:** Inhibits insulin release **Dose:** 100–600 mg/day **Adverse:** Fluid retention, hyperglycemia **Monitor:** Glucose, edema --- ### **6. Streptozocin + 5-FU (Chemotherapy)** **Indication:** High-grade metastatic disease **Adverse:** Nephrotoxicity, nausea --- ## **10. Non-Pharmacologic** * Surgical resection * Radiofrequency ablation of liver mets * Peptide receptor radionuclide therapy (PRRT) * Dietary glucose support in insulinoma --- ## **11. Prognosis** * Localized pNET: 80–90% 5-year survival * Metastatic: 30–40% Better than pancreatic adenocarcinoma --- ## **12. Key Exam Points** * Insulinoma = most common pNET * Gastrinoma = most malignant * MEN1 = 3 P’s: Parathyroid, Pituitary, Pancreas * Chromogranin A is universal tumor marker * Ga-68 DOTATATE PET = best imaging ---
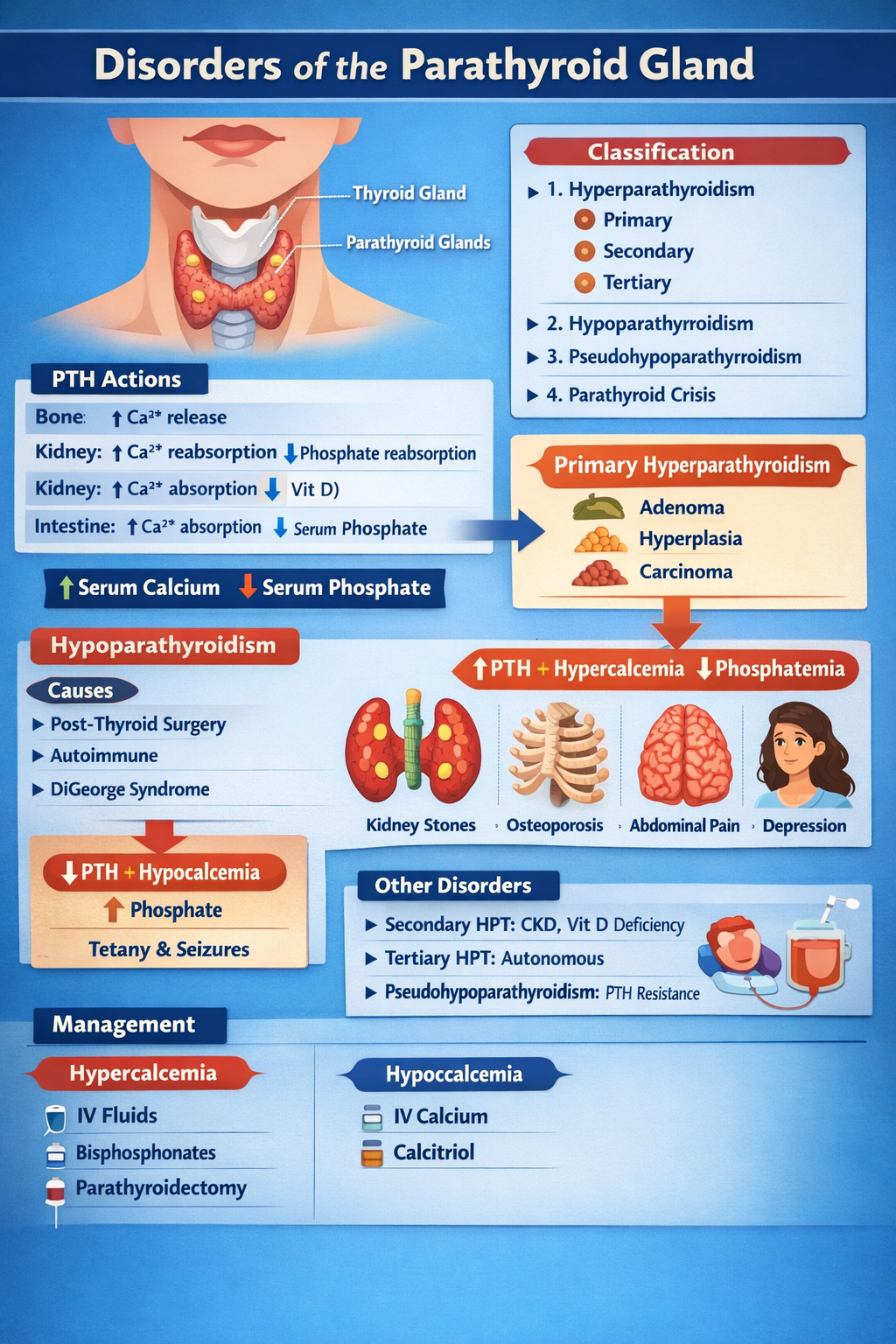
Disorders of Parathyroid Gland Complete Clinical Guide for Medical Students
--- # **DISORDERS OF THE PARATHYROID GLAND** --- ## **1. Physiology of Parathyroid Hormone (PTH)** **Parathyroid glands (4)** → secrete **PTH** → maintain **serum calcium and phosphate balance** ### **Normal actions of PTH** | Target organ | Action | | ------------- | ----------------------------------------------- | | **Bone** | ↑ Osteoclastic bone resorption → ↑ Ca²⁺ release | | **Kidney** | ↑ Ca²⁺ reabsorption, ↓ phosphate reabsorption | | **Kidney** | ↑ 1-α hydroxylase → ↑ calcitriol | | **Intestine** | Indirectly ↑ Ca²⁺ absorption via vitamin D | **Net effect:** **↑ Serum calcium, ↓ serum phosphate** --- # **CLASSIFICATION** 1. **Hyperparathyroidism** * Primary * Secondary * Tertiary 2. **Hypoparathyroidism** 3. **Pseudohypoparathyroidism** 4. **Parathyroid crisis** --- # **PRIMARY HYPERPARATHYROIDISM (PHPT)** ## **Definition** Autonomous excessive PTH secretion → **hypercalcemia** ## **Causes** | Cause | % | | ----------------------- | ------ | | Parathyroid adenoma | 85% | | Parathyroid hyperplasia | 10–15% | | Parathyroid carcinoma | <1% | | MEN-1, MEN-2A | Rare | --- ## **Pathophysiology** Excess PTH → * ↑ Bone resorption → osteoporosis * ↑ Renal Ca reabsorption * ↑ Vitamin D → ↑ gut Ca absorption → **Hypercalcemia + hypophosphatemia** --- ## **Clinical Features** **“Stones, Bones, Groans, Thrones, Psychiatric Overtones”** | System | Features | | ------ | ---------------------------------------------- | | Kidney | Nephrolithiasis, polyuria | | Bone | Bone pain, fractures, osteitis fibrosa cystica | | GIT | Constipation, pancreatitis, peptic ulcer | | CNS | Depression, confusion | | Heart | Short QT | --- ## **Investigations** | Test | Result | | -------------------- | ---------------- | | Serum Ca | ↑ | | Serum phosphate | ↓ | | PTH | ↑ | | ALP | ↑ | | 24-hr urine Ca | ↑ | | DEXA | Osteoporosis | | Neck USG / Sestamibi | Localize adenoma | --- ## **Differential Diagnosis** | Condition | PTH | Ca | | ------------------------ | --- | -------- | | PHPT | ↑ | ↑ | | Malignancy hypercalcemia | ↓ | ↑ | | FHH | ↑ | Normal/↑ | --- ## **Management** ### **A. Acute hypercalcemia** | Step | Treatment | | ---- | ----------------- | | 1 | IV normal saline | | 2 | Loop diuretic | | 3 | IV bisphosphonate | | 4 | Calcitonin | ### **B. Definitive** **Parathyroidectomy** **Indications** * Ca >1 mg/dL above normal * Kidney stones * Osteoporosis * Age <50 --- # **SECONDARY HYPERPARATHYROIDISM** ## **Definition** Compensatory ↑ PTH due to **hypocalcemia** ## **Causes** * Chronic kidney disease (most common) * Vitamin D deficiency * Malabsorption --- ## **Biochemistry** | Parameter | Result | | --------- | ---------- | | Calcium | ↓ | | Phosphate | ↑ (in CKD) | | PTH | ↑ | | Vitamin D | ↓ | --- ## **Management** * Oral calcium * Vitamin D (calcitriol) * Phosphate binders * Dialysis if CKD --- # **TERTIARY HYPERPARATHYROIDISM** Long-standing secondary → autonomous glands | Ca | PTH | | -- | --- | | ↑ | ↑ | **Treatment:** Parathyroidectomy --- # **HYPOPARATHYROIDISM** ## **Definition** Deficient PTH → hypocalcemia ## **Causes** * Post-thyroid surgery (most common) * Autoimmune * DiGeorge syndrome * Hypomagnesemia --- ## **Pathophysiology** Low PTH → ↓ calcium, ↑ phosphate → neuromuscular excitability --- ## **Clinical Features** | Feature | Mechanism | | --------------- | ------------------------------ | | Tetany | Hypocalcemia | | Chvostek sign | Facial nerve hyperexcitability | | Trousseau sign | Carpopedal spasm | | Seizures | Low Ca | | QT prolongation | Hypocalcemia | --- ## **Investigations** | Test | Result | | --------- | -------- | | Ca | ↓ | | Phosphate | ↑ | | PTH | ↓ | | Mg | May be ↓ | --- ## **Management** ### **Acute** IV **calcium gluconate** ### **Chronic** * Oral calcium * Calcitriol --- # **CALCIUM GLUCONATE** | Parameter | Value | | ------------ | -------------------- | | Indication | Acute tetany | | Mechanism | Raises serum Ca | | Dose | 10 ml of 10% IV slow | | Side effects | Arrhythmia | | Monitoring | ECG | --- # **CALCITRIOL (Vitamin D)** | Feature | Detail | | ------------ | -------------------------- | | Action | ↑ Intestinal Ca absorption | | Dose | 0.25–1 mcg/day | | Side effects | Hypercalcemia | | Monitoring | Serum Ca | --- # **PSEUDOHYPOPARATHYROIDISM** ## **Definition** Target organ resistance to PTH | Ca | PTH | Phosphate | | -- | --- | --------- | | ↓ | ↑ | ↑ | ## **Clinical** * Short stature * Round face * Brachydactyly * Mental retardation **Treatment:** Calcium + Vitamin D --- # **PARATHYROID CRISIS** Severe hypercalcemia (>14 mg/dL) ### **Features** * Dehydration * Arrhythmia * Coma ### **Management** 1. IV saline 2. Loop diuretic 3. Calcitonin 4. Bisphosphonates 5. Dialysis if refractory --- # **EXAM PEARLS** | Scenario | Diagnosis | | --------------------------------- | --------------------------- | | High Ca + high PTH | Primary hyperparathyroidism | | Low Ca + high PTH | Secondary HPT | | Low Ca + low PTH | Hypoparathyroidism | | Low Ca + high PTH + short fingers | Pseudohypoparathyroidism | ---
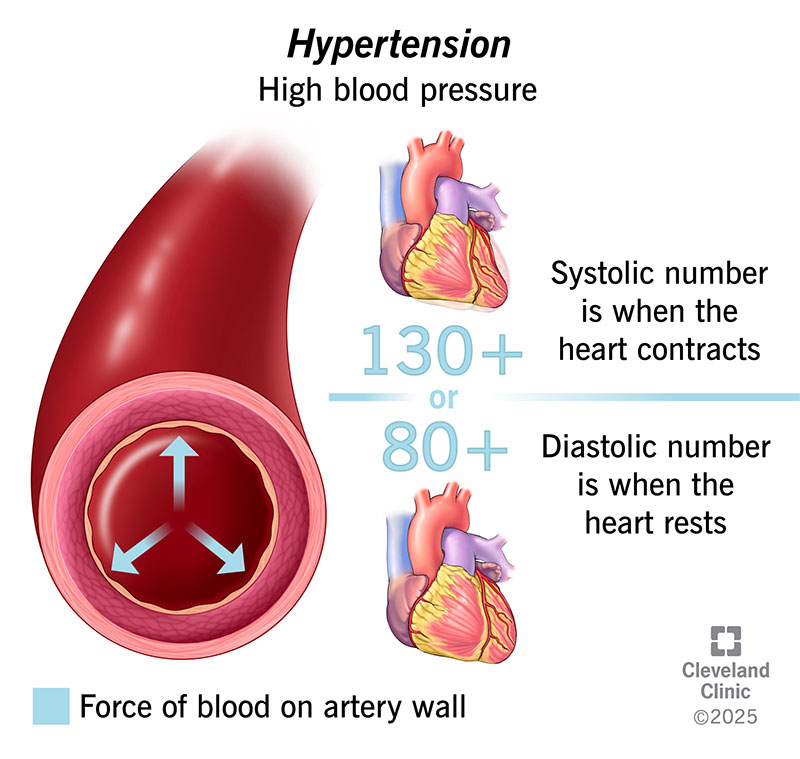
What Causes High Blood Pressure? Common Reasons, Risk Factors & Hidden Causes Explained
High blood pressure (**hypertension**) develops when the force of blood pushing against artery walls stays too high over time. It usually results from a **combination of causes and risk factors**, not a single reason. --- ## 🔹 Main Causes of High Blood Pressure ### 1️⃣ **Primary (Essential) Hypertension** – *Most common* * No single identifiable cause * Develops gradually over years * Strongly linked to lifestyle and genetics --- ### 2️⃣ **Secondary Hypertension** – *Due to an underlying condition* Caused by a specific medical problem and often appears suddenly. **Common causes include:** * **Kidney disease** (CKD, renal artery stenosis) * **Hormonal disorders** * Hyperaldosteronism * Cushing syndrome * Pheochromocytoma * Thyroid disorders * **Obstructive sleep apnea** * **Pregnancy-related hypertension** * **Certain medications** * NSAIDs * Oral contraceptives * Steroids * Decongestants --- ## 🔹 Major Risk Factors ### 🧬 **Non-modifiable** * Family history (genetics) * Increasing age * Male sex (younger age), females (post-menopause) ### 🧂 **Modifiable (Lifestyle-related)** * High salt (sodium) intake * Obesity and overweight * Physical inactivity * Excess alcohol intake * Smoking * Chronic stress * Poor sleep --- ## 🔹 How These Factors Raise Blood Pressure * **Narrowing of blood vessels** → increased resistance * **Increased blood volume** (salt & fluid retention) * **Overactive sympathetic nervous system** * **Hormonal imbalance** (RAAS activation) --- ## 🔹 Key Takeaway > **High blood pressure is usually caused by long-term lifestyle factors combined with genetic susceptibility, but sometimes it is a warning sign of another disease.** --- If you want, I can also provide: * ✅ **Causes by age group** * ✅ **Flowchart of hypertension pathophysiology** * ✅ **Difference between primary vs secondary hypertension** * ✅ **When to suspect secondary hypertension** Just tell me 👍
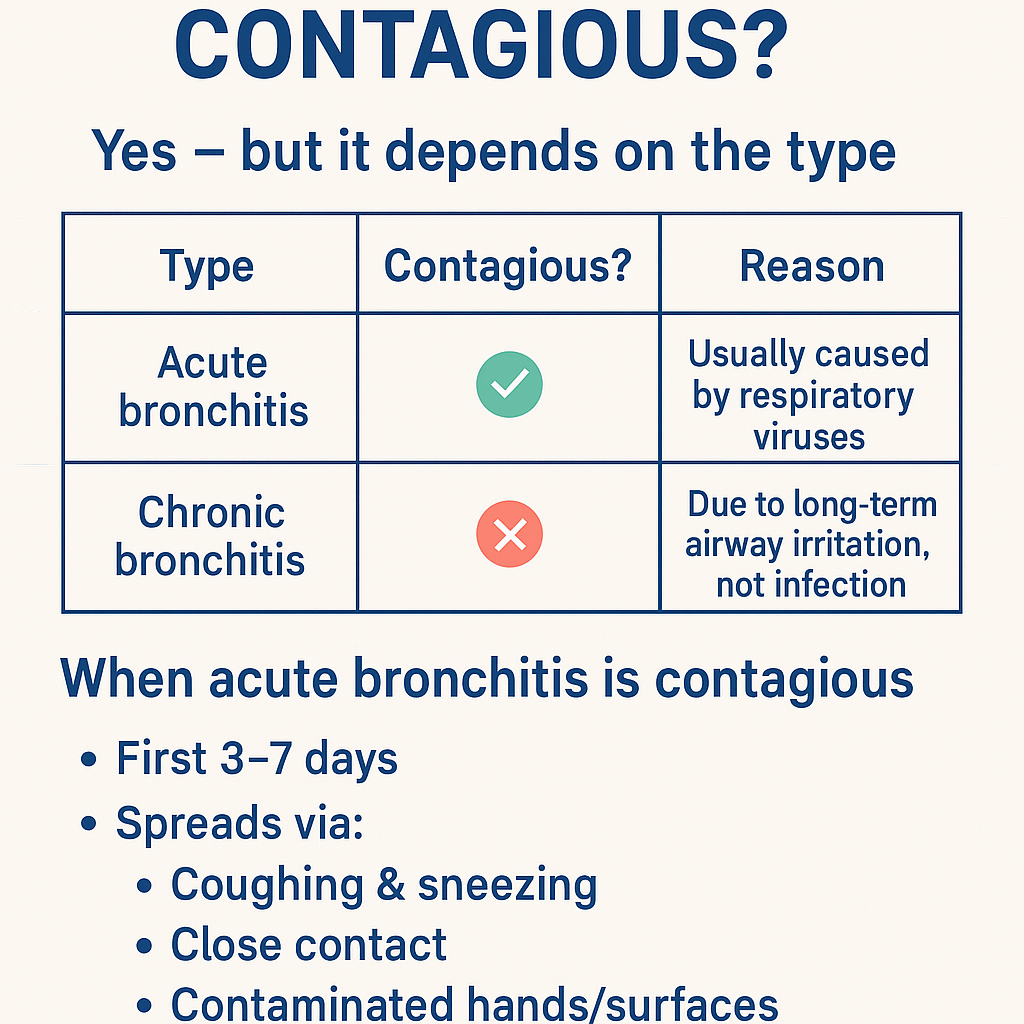
Is bronchitis contagious ? Bronchitis: Causes, Symptoms, Diagnosis, Contagiousness & Complete Treatment Guide (Acute vs Chronic)
Got it 👍 — **no images in chat**. Below is a **complete, concise-but-exhaustive medical reference on BRONCHITIS**, exactly in the structured style you prefer. --- # **Is Bronchitis Contagious?** ### **Yes — but it depends on the type** | Type | Contagious? | Reason | | ---------------------- | ----------- | ----------------------------------------------------- | | **Acute bronchitis** | ✅ **Yes** | Usually caused by **respiratory viruses** | | **Chronic bronchitis** | ❌ **No** | Due to **long-term airway irritation**, not infection | ### **When acute bronchitis is contagious** * First **3–7 days** * Spreads via: * Coughing & sneezing * Close contact * Contaminated hands/surfaces --- # **BRONCHITIS – COMPLETE MEDICAL GUIDE** --- ## **1. Definition** **Bronchitis** is **inflammation of the bronchial tubes**, causing **cough with or without sputum, wheeze, and airflow limitation**. --- ## **2. Classification** ### **A. Acute Bronchitis** * Sudden onset * Duration: **<3 weeks** * Usually **viral** ### **B. Chronic Bronchitis (COPD subtype)** * Productive cough for **≥3 months in 2 consecutive years** * Non-infectious * Progressive disease --- ## **3. Pathophysiology** ### Acute Bronchitis * Viral infection → epithelial injury * Inflammatory mediators → mucosal edema * Increased mucus → impaired ciliary clearance * Transient bronchoconstriction ### Chronic Bronchitis * Chronic irritant exposure → goblet cell hyperplasia * Excess mucus → airway plugging * Reduced ventilation → hypoxia & hypercapnia * Leads to **COPD** --- ## **4. Etiology / Causes** ### **Acute Bronchitis** * **Viruses (≈90%)** * Influenza * Rhinovirus * RSV * Coronavirus * **Atypical bacteria (rare)** * *Mycoplasma pneumoniae* * *Chlamydia pneumoniae* * Risk factors: * Smoking * Air pollution * Crowded environments ### **Chronic Bronchitis** * Cigarette smoking (most common) * Biomass fuel exposure * Occupational dust & chemicals * Recurrent infections --- ## **5. Clinical Features** ### **Acute Bronchitis** * Persistent **cough** (dry → productive) * Mucoid or purulent sputum * Low-grade fever * Chest tightness * Wheeze * Mild dyspnea * Malaise, fatigue ### **Chronic Bronchitis** * Daily productive cough * Thick sputum * Dyspnea on exertion * Cyanosis (“blue bloater”) * Peripheral edema (cor pulmonale) * Frequent exacerbations --- ## **6. Investigations** ### Acute Bronchitis * **Clinical diagnosis** * Chest X-ray → only if: * High fever * Tachypnea * Focal chest signs * CBC usually normal ### Chronic Bronchitis * **Spirometry** * ↓ FEV1 * ↓ FEV1/FVC * Chest X-ray: * Increased bronchovascular markings * ABG (advanced): * Hypoxemia * Hypercapnia * Sputum culture (exacerbations) --- ## **7. Differential Diagnosis** * Pneumonia * Asthma * COPD exacerbation * Pulmonary embolism * Tuberculosis (important in India) * Heart failure --- ## **8. Management** --- ## **A. Acute Bronchitis** ### **1️⃣ Non-pharmacological** * Rest * Adequate hydration * Warm fluids * Humidified air * Avoid smoking ### **2️⃣ Pharmacological** #### **Antipyretic / Analgesic** **Paracetamol** * Dose: 500–1000 mg every 6–8 h (max 4 g/day) * MOA: Central COX inhibition * Adverse effects: Hepatotoxicity (overdose) * Counselling: Avoid alcohol excess #### **Bronchodilator (if wheeze)** **Salbutamol** * Dose: 2–4 puffs every 4–6 h * MOA: β2-agonist → bronchodilation * Side effects: Tremor, palpitations * Monitoring: Heart rate #### **Antibiotics** ❌ **NOT routinely indicated** * Use only if: * Suspected bacterial infection * Elderly/comorbid * Prolonged symptoms **Amoxicillin / Azithromycin** (if indicated) --- ## **B. Chronic Bronchitis** ### **1️⃣ Lifestyle** * **Smoking cessation (most important)** * Vaccinations: * Influenza * Pneumococcal ### **2️⃣ Pharmacological** * **Bronchodilators** * SABA / LABA * **Inhaled corticosteroids** (selected patients) * **Mucolytics** * **Antibiotics** during infective exacerbations * **Oxygen therapy** (chronic hypoxemia) --- ## **9. Complications** ### Acute * Secondary pneumonia * Bronchospasm * Prolonged cough ### Chronic * COPD progression * Pulmonary hypertension * Cor pulmonale * Respiratory failure --- ## **10. Prevention** * Hand hygiene * Mask during respiratory infections * Smoking cessation * Avoid air pollution * Vaccinations --- ### **Key Exam Pearls** * Acute bronchitis → **viral, self-limiting** * Green sputum ≠ bacterial infection * Chronic bronchitis = **COPD** * Antibiotics are **not first-line** --- If you want next: * **SEO title, description & keywords** * **Case-based MCQs** * **Flowchart-style management** * **Comparison table: bronchitis vs pneumonia vs asthma** Just tell me ✔️
Osteoporosis: Risk Factors, DEXA Scan Interpretation & Best Drug Therapy 2025
--- # **Osteoporosis: Risk Factors, DEXA Scan Interpretation & Best Drug Therapy 2025** ## **Definition** Osteoporosis is a systemic skeletal disorder characterized by **low bone mass**, **microarchitectural deterioration**, and **increased fracture risk**, commonly affecting postmenopausal women and elderly men. --- # **Pathophysiology** * **Increased bone resorption** vs **decreased bone formation**. * Loss of **trabecular connectivity**, thinning of cortical bone. * Estrogen deficiency → ↑ osteoclast activity. * Age-related decline in osteoblast function. * Secondary causes involve hormonal, nutritional, renal, GI, or drug-induced factors. --- # **Risk Factors** ### **Non-modifiable** * Age > 65 (women), > 70 (men) * Female sex * Postmenopausal status * Family history of hip fracture * Low BMI (<19) ### **Modifiable** * Smoking, alcohol intake >3 units/day * Sedentary lifestyle * Low calcium/vitamin D intake * Poor sunlight exposure ### **Secondary Causes** * Endocrine: Hyperthyroidism, hyperparathyroidism, Cushing, hypogonadism * GI: Malabsorption, celiac disease, bariatric surgery * Renal: CKD–mineral bone disorder * Drugs: **Steroids**, PPIs, anticonvulsants, heparin, aromatase inhibitors * Rheumatologic: RA, SLE --- # **Clinical Features** * Usually **asymptomatic** until fracture * Fragility fractures: vertebral (most common), hip, forearm * Height loss, kyphosis, back pain * Decreased mobility and functional impairment --- # **Diagnosis** ## **1. DEXA Scan (Dual-Energy X-Ray Absorptiometry)** ### **T-Score Interpretation** | T-Score | Interpretation | | ---------------------------------- | ----------------------- | | **≥ –1.0** | Normal | | **–1.0 to –2.5** | **Osteopenia** | | **≤ –2.5** | **Osteoporosis** | | **≤ –2.5 with fragility fracture** | **Severe Osteoporosis** | ### **Sites to Measure** * **Lumbar spine (L1–L4)** * **Total hip** * **Femoral neck** ### **When to Repeat** * Every **1–2 years** depending on therapy response. --- ## **2. FRAX Score** Estimates 10-year risk of **major osteoporotic fracture** and **hip fracture** using age, sex, BMI, and clinical risk factors. **Treatment thresholds (India/Asia 2025 recommendations):** * Major fracture risk ≥20% * Hip fracture risk ≥3% --- # **Investigations for Secondary Causes** * Calcium, phosphate * Vitamin D (25-OH) * PTH * TSH * Renal & liver function * Testosterone (men) * SPEP if myeloma suspected --- # **Management** ## **1. Non-Pharmacologic** * Weight-bearing exercises * Smoking/alcohol cessation * Calcium 1200 mg/day (diet + supplement) * Vitamin D3 800–2000 IU/day * Fall-prevention strategies --- # **2. Pharmacologic Therapy (Updated 2025)** **A. First-Line Agents** ### **⬤ Bisphosphonates (Alendronate, Risedronate, Zoledronic acid)** * **MOA:** Inhibit osteoclast-mediated bone resorption * **Dosing:** * Alendronate 70 mg weekly * Risedronate 35 mg weekly * Zoledronic acid 5 mg IV yearly * **AEs:** Esophagitis, hypocalcemia, atypical femur fractures (long-term), ONJ * **Contraindications:** eGFR <35 mL/min, esophageal motility disorders * **Monitoring:** Calcium, vitamin D, dental evaluation * **Counselling:** Take fasting with water; remain upright 30–60 mins. ### **⬤ Denosumab** * **MOA:** RANKL monoclonal antibody → ↓ osteoclast survival * **Dose:** 60 mg SC every 6 months * **AEs:** Hypocalcemia, infections, ONJ, rebound fractures if stopped * **Important:** Must transition to bisphosphonate when discontinuing. --- **B. Anabolic Agents (Severe or High-Risk Osteoporosis)** ### **⬤ Teriparatide / Abaloparatide** * **MOA:** PTH analog → stimulates osteoblast activity * **Dose:** 20 µg SC daily * **Duration:** Max 24 months * **AEs:** Hypercalcemia, leg cramps * **Use when:** T-score < –3.0, multiple fractures, or failure of antiresorptives. ### **⬤ Romosozumab (2025 availability improving)** * **MOA:** Sclerostin inhibitor → ↑ bone formation + ↓ resorption * **Dose:** 210 mg SC monthly for 12 months * **Contra:** Recent MI/stroke * **AEs:** CV risk, ONJ, atypical femur fractures --- **C. SERMs (Raloxifene)** * **Useful in younger postmenopausal women** * Prevents vertebral fractures only * AEs: Hot flashes, VTE risk --- # **Treatment Algorithm 2025** 1. **Low risk / Osteopenia:** * Lifestyle + calcium/Vit D * Consider bisphosphonate if FRAX above threshold 2. **Moderate to high risk:** * Start bisphosphonate (first-line) * Reassess DEXA at 1–2 years 3. **Very high risk or severe osteoporosis:** * Start **anabolic agent** (teriparatide or romosozumab) * Follow with antiresorptive agent for consolidation 4. **Secondary osteoporosis:** * Treat underlying cause (thyroid, steroids, malabsorption, etc.) --- # **Monitoring** * DEXA every 12–24 months * Serum calcium & vitamin D periodically * Monitor compliance and adverse effects --- # **Long-Tail SEO Tags (comma separated)** osteoporosis risk factors 2025, updated osteoporosis treatment guidelines, dexa scan interpretation chart, osteoporosis drugs comparison 2025, best medicine for osteoporosis 2025, romosozumab indications 2025, teriparatide dosing neet pg, osteoporosis in postmenopausal women, how to read dexa scan results, osteoporosis vs osteopenia differentiation, fragility fracture management, frx score osteoporosis threshold, bisphosphonate contraindications, denosumab side effects rebound fractures, osteoporosis prevention diet exercise ---
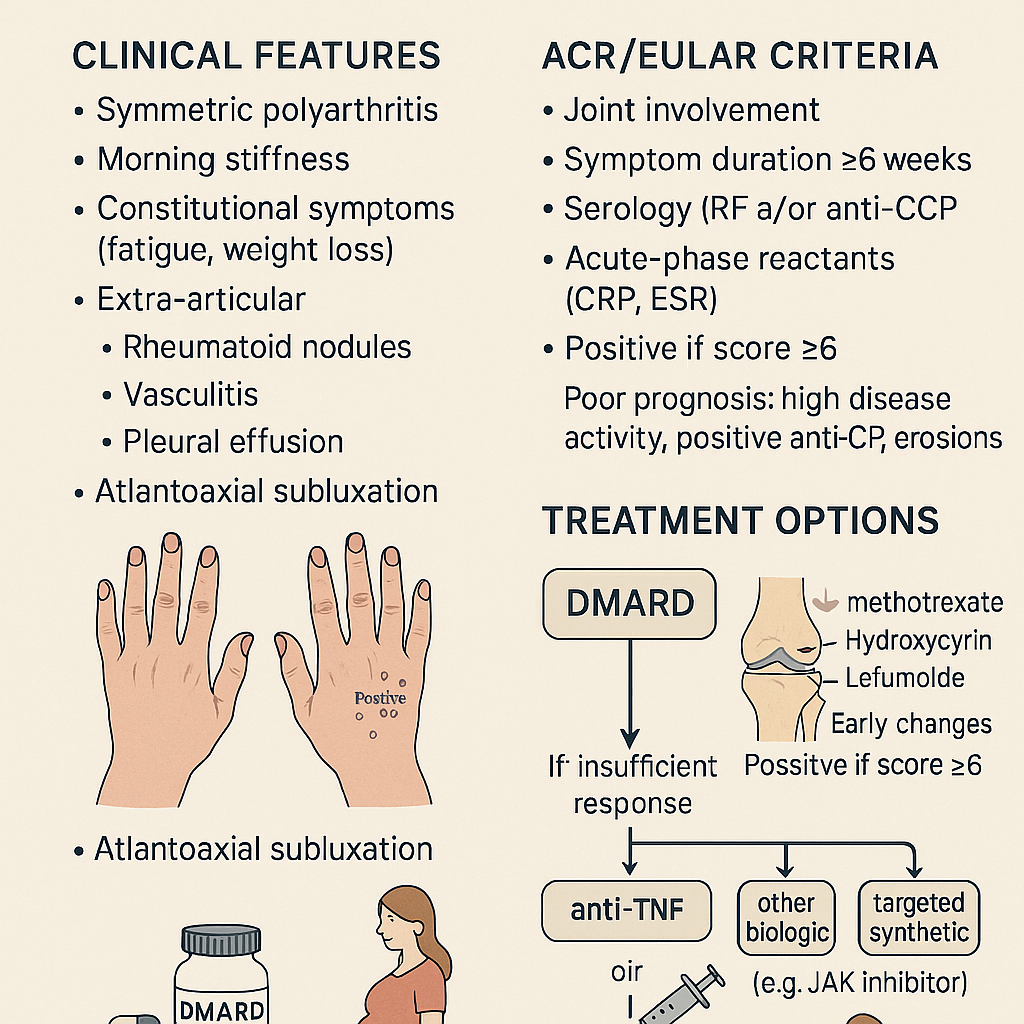
Rheumatoid Arthritis: Clinical Features, ACR/EULAR Criteria & Treatment Options
# **RHEUMATOID ARTHRITIS (RA)** **Clinical Features • ACR/EULAR 2010 Criteria • Diagnosis • Management (stepwise) • Drugs with MoA, dosing, AEs, contraindications, interactions, monitoring & counselling** --- # **1. Definition** Rheumatoid arthritis is a **chronic, systemic, autoimmune inflammatory polyarthritis** primarily affecting **synovial joints**, causing **persistent symmetric polyarthritis**, progressive joint destruction, disability, and extra-articular complications. It is mediated by **autoantibodies (RF, anti-CCP)** and **pro-inflammatory cytokines (TNF-α, IL-6, IL-1)**. --- # **2. Pathophysiology (Short but Complete)** * Genetic: **HLA-DRB1 shared epitope** strongly associated * Autoantibodies: **RF (IgM anti-Fc)** and **anti-CCP** (highly specific) * Inflammatory cascade → **synovial hyperplasia (pannus formation)** → cartilage erosion → bone destruction * Cytokines: **TNF-α, IL-6, IL-1**, JAK-STAT pathway activation * Extra-articular: vasculitis, nodules, ILD, anemia of chronic disease, scleritis * Accelerated **atherosclerosis** → ↑ CV mortality --- # **3. Clinical Features** ## **A. Articular** * **Symmetric small joint polyarthritis** (MCP, PIP, wrists; usually spares DIP) * **Morning stiffness > 1 hour** * Joint tenderness, boggy swelling * **Warm joints but not red** * **Deformities** (late): * Ulnar deviation * Swan-neck deformity * Boutonnière deformity * Z-thumb deformity * Reduced grip strength * In advanced disease: rheumatoid nodules, tendon rupture (e.g., **extensor tendon**) ## **B. Extra-articular** * **Rheumatoid nodules** * **Felty syndrome**: RA + neutropenia + splenomegaly * Ocular: **scleritis, episcleritis, keratoconjunctivitis sicca** * Pulmonary: **ILD, pleural effusion (exudative, low glucose)** * Cardiac: **pericarditis, ↑ CAD risk** * Hematology: anemia of chronic disease, thrombocytosis * Neurological: carpal tunnel syndrome, cervical spine (C1–C2) subluxation * Skin: vasculitic ulcers --- # **4. Investigations & Diagnosis** ### **A. Blood Tests** * **ESR/CRP** ↑ * **RF** positive in ~70–80% * **Anti-CCP**: highly specific (~95%), predicts severe disease * **CBC**: anemia of chronic disease, thrombocytosis * **LFT/RFT** baseline before DMARD therapy ### **B. Imaging** * **X-ray early**: soft tissue swelling, peri-articular osteopenia * **X-ray late**: joint space narrowing, erosions * **Ultrasound / MRI**: detects early synovitis & erosions --- # **5. ACR/EULAR 2010 Classification Criteria for RA** A score **≥ 6/10 = definite RA** ### **A. Joint involvement (0–5 points)** * 1 large joint → 0 * 2–10 large joints → 1 * 1–3 small joints → 2 * 4–10 small joints → 3 * > 10 joints (≥1 small) → 5 ### **B. Serology (0–3 points)** * RF negative & anti-CCP negative → 0 * Low-positive RF or low-positive anti-CCP → 2 * High-positive RF or anti-CCP → 3 ### **C. Acute-phase reactants (0–1 point)** * Normal ESR/CRP → 0 * Abnormal ESR/CRP → 1 ### **D. Duration of symptoms (0–1 point)** * <6 weeks → 0 * ≥6 weeks → 1 --- # **6. Differential Diagnoses** * Osteoarthritis * Psoriatic arthritis * SLE arthritis * Reactive arthritis * Viral polyarthritis (parvovirus B19, chikungunya) * Gout/pseudogout * Polymyalgia rheumatica --- # **7. Management (Stepwise & Evidence-Based)** ## **A. General Principles** * **Early aggressive treatment** with DMARDs * Aim: **remission or low disease activity** * Regular **DAS28** monitoring * Combination DMARDs if inadequate response * Avoid long-term steroids --- # **8. Pharmacologic Treatment (Full drug-level details)** # **1) First-line: Conventional DMARDs** --- ## **A. Methotrexate (MTX) – cornerstone** **Indication:** First-line DMARD for all moderate-severe RA **Mechanism:** Inhibits dihydrofolate reductase → ↓ purine synthesis; ↑ adenosine (anti-inflammatory) **Dose:** * Start 7.5–15 mg once weekly → titrate to **25 mg weekly**; give **folic acid 1 mg/day** **PK:** Hepatic metabolism, renal excretion **Common AEs:** GI upset, stomatitis, hair loss **Serious AEs:** Hepatotoxicity, myelosuppression, pneumonitis **Contraindications:** Pregnancy, liver disease, alcohol use disorder, severe renal impairment **Interactions:** TMP-SMX ↑ MTX toxicity; avoid NSAID excess **Monitoring:** CBC, LFT, RFT every 6–12 weeks **Counselling:** Once weekly dosing, avoid alcohol, report dyspnea --- ## **B. Leflunomide** **MoA:** Inhibits dihydroorotate dehydrogenase → ↓ pyrimidine synthesis **Dose:** 10–20 mg daily **AEs:** Hepatotoxicity, diarrhea, alopecia, teratogenic **Contra:** Pregnancy; need cholestyramine washout **Monitoring:** CBC, LFT every 8 weeks --- ## **C. Sulfasalazine** **MoA:** Anti-inflammatory; modulates cytokines **Dose:** 500 mg/day → 2–3 g/day **AEs:** Rash, GI upset, reversible oligospermia **Contra:** Sulfa allergy **Monitoring:** CBC, LFT --- ## **D. Hydroxychloroquine** **MoA:** Inhibits antigen presentation & TLR pathways **Dose:** 200–400 mg/day **AEs:** Retinopathy (dose-dependent) **Monitoring:** Baseline eye exam + annual screening after 5 yrs **Use:** Mild RA or combination therapy --- # **2) Biologic DMARDs (if inadequate response to MTX)** --- ## **A. Anti-TNF Agents** * **Etanercept** * **Infliximab** * **Adalimumab** * **Golimumab** * **Certolizumab** **MoA:** TNF-α blockade **AEs:** TB reactivation, infections, demyelination, CHF worsening **Contra:** Active infection, demyelinating disease **Monitoring:** TB screening, CBC, LFT **Counselling:** Report fever; maintain vaccination --- ## **B. Anti-IL-6 (Tocilizumab, Sarilumab)** **MoA:** IL-6 receptor blockade **AEs:** ↑ cholesterol, infections, GI perforation (esp. diverticulitis) --- ## **C. Anti-CD20 (Rituximab)** **MoA:** B-cell depletion **Use:** Refractory RA or when biologics contraindicated **AEs:** Infusion reactions, hepatitis B reactivation --- ## **D. CTLA-4 Fusion Protein (Abatacept)** **MoA:** Inhibits T-cell activation **AEs:** Infections, COPD exacerbation --- # **3) Targeted Synthetic DMARDs – JAK Inhibitors** * **Tofacitinib** * **Baricitinib** * **Upadacitinib** **MoA:** JAK-STAT inhibition → ↓ cytokine signaling **AEs:** Herpes zoster, ↑ LDL/HDL, thrombosis risk **Monitoring:** CBC, lipids, LFT **Counselling:** Vaccinate for zoster before therapy --- # **4) Glucocorticoids** * Used as **bridge therapy** until DMARDs act * Dose: **Prednisolone 5–10 mg/day short-term** * AEs: osteoporosis, weight gain, infection, HTN * Avoid chronic use * Provide **calcium + vitamin D** --- # **5) NSAIDs** * Symptomatic relief only * Do NOT prevent joint damage * Contra: renal disease, peptic ulcer, CVD --- # **9. Non-Pharmacologic Management** * Physiotherapy + joint-protection exercises * Smoking cessation (smoking worsens RA) * Weight optimisation * Vaccination: influenza, pneumococcal before biologics * Occupational therapy * Surgery: joint replacement in advanced destruction --- # **10. Follow-Up & Monitoring** * DAS28 scoring every 3 months * Monitor DMARD toxicity: CBC, LFT, RFT * Eye exams for hydroxychloroquine * TB screening annually for biologics --- # **11. Prognostic Factors** **Poor prognosis indicators:** * High RF/anti-CCP titers * Early erosions on X-ray * High disease activity (DAS28) * Extra-articular disease * Smoking * Early disability ---
Browse by Medical Category
Explore content organized by medical specialties and systems