Clinical videos + HTML notes for NEET PG-ready revision.
Streamora lets you upload case-based videos, attach rich HTML notes, like and comment on other clinicians’ posts, follow creators and save structured exam-oriented pearls – all mobile-first and SEO-ready.
Why Streamora stands out for NEET PG aspirants: Unlike generic apps, we focus on high-yield topics like labour stages (from first to fourth, with management pitfalls), Rh-negative pregnancies (anti-D prophylaxis timing), and anatomy pearls (e.g., sacral hiatus for caudal blocks). Our community-driven notes include real residency cases—e.g., "Missed Rh isoimmunization leading to hydrops fetalis"—with attached flowcharts and MCQ-style tags for quick revision. Free, ad-light, and built by med students for med students.
Latest Medical Posts
High-yield medical discussions, NEET PG-flavoured notes and short clinical cases from all users.
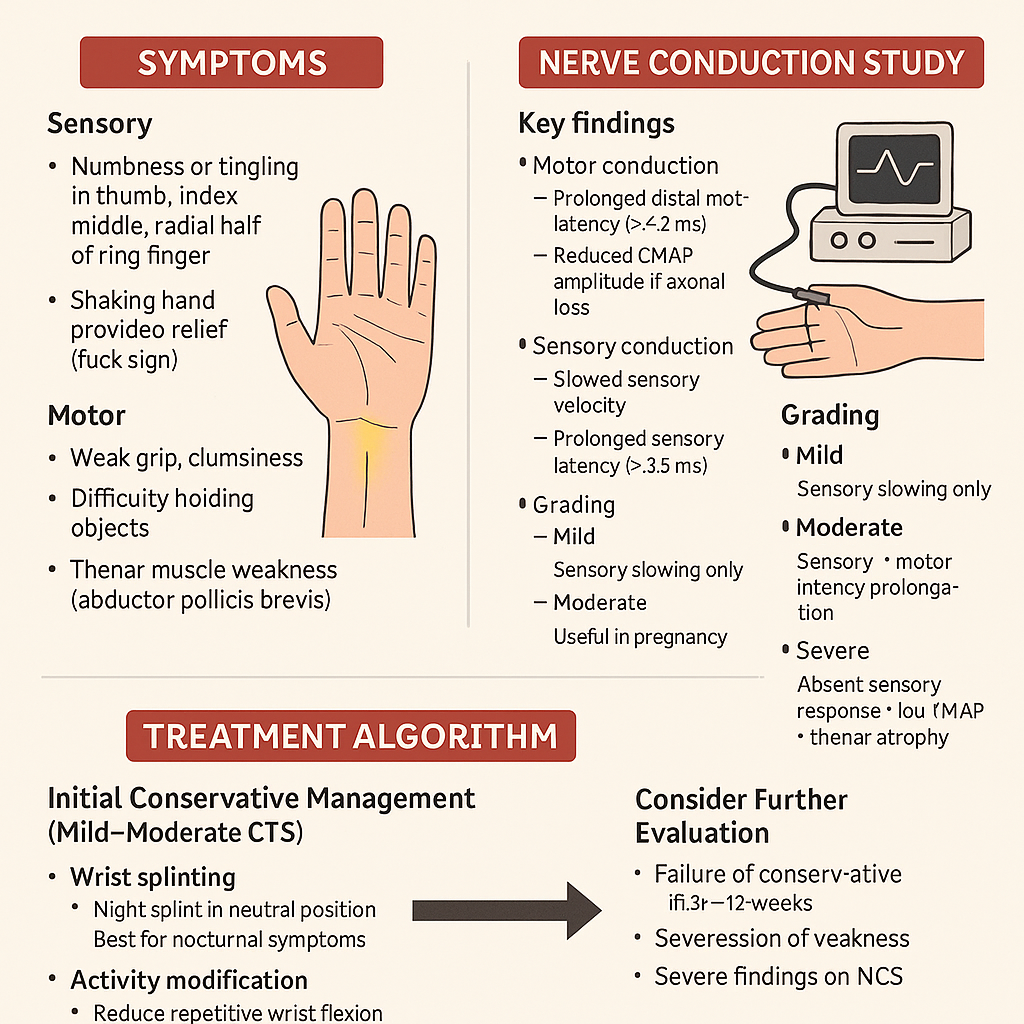
Carpal Tunnel Syndrome: Symptoms, Nerve Conduction Study & Treatment Algorithm
# **Carpal Tunnel Syndrome (CTS): Symptoms, Nerve Conduction Study & Treatment Algorithm** ## **Definition** Carpal Tunnel Syndrome is **median nerve compression** at the level of the wrist within the **carpal tunnel**, leading to sensory and motor dysfunction in the **median nerve distribution**. --- # **Pathophysiology** * The **carpal tunnel** is a rigid space bordered by carpal bones and the **transverse carpal ligament**. * Conditions causing tunnel **volume increase** or **nerve vulnerability** → median nerve ischemia + demyelination. * Chronic compression → **axonal loss** → persistent weakness and atrophy. --- # **Causes / Risk Factors** ### **Local / Mechanical** * Repetitive wrist flexion/extension * Vibrating tool use * Wrist fractures/dislocations * Ganglion cysts, synovitis ### **Systemic** * Diabetes mellitus * Hypothyroidism * Pregnancy (fluid retention) * Rheumatoid arthritis * Obesity * Amyloidosis --- # **Clinical Features** ### **Symptoms** **Sensory:** * Numbness/tingling in **thumb, index, middle, radial half of ring finger** * Symptoms worse at **night** * **Shaking hand provides relief** (flick sign) **Motor:** * Weak grip, clumsiness * Difficulty holding objects * **Thenar muscle weakness** (abductor pollicis brevis) **Autonomic signs (less common):** * Dryness of skin over lateral 3½ fingers --- ### **Physical Examination** * **Tinel’s sign:** Tapping over carpal tunnel → tingling in median nerve area * **Phalen’s test:** Forced wrist flexion for 60 sec → reproduces symptoms * **Durkan’s test (carpal compression test):** Direct pressure over the tunnel → most sensitive * Thenar muscle **atrophy** in advanced disease --- # **Nerve Conduction Study (NCS) — Key Findings** NCS is the **gold standard**. ### **Motor conduction** * Prolonged **distal motor latency** (> 4.2 ms) of median nerve * Reduced CMAP amplitude if axonal loss ### **Sensory conduction** * Slowed sensory velocity * Prolonged **sensory latency** (> 3.5 ms) * Reduced SNAP amplitude ### **Comparison tests** * Median vs ulnar sensory latency to ring finger * Median–radial latency difference to thumb * Very sensitive in early disease ### **Grading** * **Mild:** Sensory slowing only * **Moderate:** Sensory + motor latency prolongation * **Severe:** Absent sensory response + low CMAP + thenar atrophy --- # **Diagnosis** * Clinical examination + NCS * Ultrasound: Median nerve cross-sectional area > **9–10 mm²** at carpal tunnel inlet * X-ray only if trauma suspected * Rule out differentials: cervical radiculopathy (C6), pronator syndrome, diabetic polyneuropathy --- # **Treatment Algorithm (Stepwise)** ## **1. Initial Conservative Management (Mild–Moderate CTS)** ### **a. Wrist Splinting** * **Night splint** in neutral position * Best first-line for nocturnal symptoms ### **b. Activity Modification** * Reduce repetitive wrist flexion * Ergonomic adjustments ### **c. NSAIDs** * Provides symptom relief, but **does not alter nerve pathology** ### **d. Corticosteroid Injection** * Local steroid injection gives **weeks–months of relief** * Useful in pregnancy * Avoid frequent injections (>3/year) --- ## **2. Consider Further Evaluation** * Failure of conservative therapy in **6–12 weeks** * Progression of weakness * Severe findings on NCS --- ## **3. Definitive Treatment — Surgery** ### **Surgical Indication** * Persistent symptoms despite conservative therapy * Severe CTS (thenar atrophy or axonal loss on NCS) * Recurrent symptoms significantly affecting function ### **Procedure** **Carpal Tunnel Release (CTR)** * Cut the transverse carpal ligament to decompress the median nerve * Approaches: **open** or **endoscopic** ### **Outcomes** * Excellent symptom improvement in majority * Thenar strength recovery depends on duration of compression * Recurrence is uncommon --- # **Prognosis** * Early-stage CTS responds well to conservative therapy * Long-standing compression with axonal damage → incomplete recovery * Diabetes: slower improvement * Pregnancy: symptoms often resolve postpartum --- # **Red Flags (Suggest Alternative Diagnosis)** * Whole-hand numbness (not median distribution) * Neck pain + hand paresthesia → cervical radiculopathy * Symptoms not affected by wrist position * Marked weakness without sensory loss → motor neuron or peripheral nerve disorder ---
Osteoporosis: Risk Factors, DEXA Scan Interpretation & Best Drug Therapy 2025
--- # **Osteoporosis: Risk Factors, DEXA Scan Interpretation & Best Drug Therapy 2025** ## **Definition** Osteoporosis is a systemic skeletal disorder characterized by **low bone mass**, **microarchitectural deterioration**, and **increased fracture risk**, commonly affecting postmenopausal women and elderly men. --- # **Pathophysiology** * **Increased bone resorption** vs **decreased bone formation**. * Loss of **trabecular connectivity**, thinning of cortical bone. * Estrogen deficiency → ↑ osteoclast activity. * Age-related decline in osteoblast function. * Secondary causes involve hormonal, nutritional, renal, GI, or drug-induced factors. --- # **Risk Factors** ### **Non-modifiable** * Age > 65 (women), > 70 (men) * Female sex * Postmenopausal status * Family history of hip fracture * Low BMI (<19) ### **Modifiable** * Smoking, alcohol intake >3 units/day * Sedentary lifestyle * Low calcium/vitamin D intake * Poor sunlight exposure ### **Secondary Causes** * Endocrine: Hyperthyroidism, hyperparathyroidism, Cushing, hypogonadism * GI: Malabsorption, celiac disease, bariatric surgery * Renal: CKD–mineral bone disorder * Drugs: **Steroids**, PPIs, anticonvulsants, heparin, aromatase inhibitors * Rheumatologic: RA, SLE --- # **Clinical Features** * Usually **asymptomatic** until fracture * Fragility fractures: vertebral (most common), hip, forearm * Height loss, kyphosis, back pain * Decreased mobility and functional impairment --- # **Diagnosis** ## **1. DEXA Scan (Dual-Energy X-Ray Absorptiometry)** ### **T-Score Interpretation** | T-Score | Interpretation | | ---------------------------------- | ----------------------- | | **≥ –1.0** | Normal | | **–1.0 to –2.5** | **Osteopenia** | | **≤ –2.5** | **Osteoporosis** | | **≤ –2.5 with fragility fracture** | **Severe Osteoporosis** | ### **Sites to Measure** * **Lumbar spine (L1–L4)** * **Total hip** * **Femoral neck** ### **When to Repeat** * Every **1–2 years** depending on therapy response. --- ## **2. FRAX Score** Estimates 10-year risk of **major osteoporotic fracture** and **hip fracture** using age, sex, BMI, and clinical risk factors. **Treatment thresholds (India/Asia 2025 recommendations):** * Major fracture risk ≥20% * Hip fracture risk ≥3% --- # **Investigations for Secondary Causes** * Calcium, phosphate * Vitamin D (25-OH) * PTH * TSH * Renal & liver function * Testosterone (men) * SPEP if myeloma suspected --- # **Management** ## **1. Non-Pharmacologic** * Weight-bearing exercises * Smoking/alcohol cessation * Calcium 1200 mg/day (diet + supplement) * Vitamin D3 800–2000 IU/day * Fall-prevention strategies --- # **2. Pharmacologic Therapy (Updated 2025)** **A. First-Line Agents** ### **⬤ Bisphosphonates (Alendronate, Risedronate, Zoledronic acid)** * **MOA:** Inhibit osteoclast-mediated bone resorption * **Dosing:** * Alendronate 70 mg weekly * Risedronate 35 mg weekly * Zoledronic acid 5 mg IV yearly * **AEs:** Esophagitis, hypocalcemia, atypical femur fractures (long-term), ONJ * **Contraindications:** eGFR <35 mL/min, esophageal motility disorders * **Monitoring:** Calcium, vitamin D, dental evaluation * **Counselling:** Take fasting with water; remain upright 30–60 mins. ### **⬤ Denosumab** * **MOA:** RANKL monoclonal antibody → ↓ osteoclast survival * **Dose:** 60 mg SC every 6 months * **AEs:** Hypocalcemia, infections, ONJ, rebound fractures if stopped * **Important:** Must transition to bisphosphonate when discontinuing. --- **B. Anabolic Agents (Severe or High-Risk Osteoporosis)** ### **⬤ Teriparatide / Abaloparatide** * **MOA:** PTH analog → stimulates osteoblast activity * **Dose:** 20 µg SC daily * **Duration:** Max 24 months * **AEs:** Hypercalcemia, leg cramps * **Use when:** T-score < –3.0, multiple fractures, or failure of antiresorptives. ### **⬤ Romosozumab (2025 availability improving)** * **MOA:** Sclerostin inhibitor → ↑ bone formation + ↓ resorption * **Dose:** 210 mg SC monthly for 12 months * **Contra:** Recent MI/stroke * **AEs:** CV risk, ONJ, atypical femur fractures --- **C. SERMs (Raloxifene)** * **Useful in younger postmenopausal women** * Prevents vertebral fractures only * AEs: Hot flashes, VTE risk --- # **Treatment Algorithm 2025** 1. **Low risk / Osteopenia:** * Lifestyle + calcium/Vit D * Consider bisphosphonate if FRAX above threshold 2. **Moderate to high risk:** * Start bisphosphonate (first-line) * Reassess DEXA at 1–2 years 3. **Very high risk or severe osteoporosis:** * Start **anabolic agent** (teriparatide or romosozumab) * Follow with antiresorptive agent for consolidation 4. **Secondary osteoporosis:** * Treat underlying cause (thyroid, steroids, malabsorption, etc.) --- # **Monitoring** * DEXA every 12–24 months * Serum calcium & vitamin D periodically * Monitor compliance and adverse effects --- # **Long-Tail SEO Tags (comma separated)** osteoporosis risk factors 2025, updated osteoporosis treatment guidelines, dexa scan interpretation chart, osteoporosis drugs comparison 2025, best medicine for osteoporosis 2025, romosozumab indications 2025, teriparatide dosing neet pg, osteoporosis in postmenopausal women, how to read dexa scan results, osteoporosis vs osteopenia differentiation, fragility fracture management, frx score osteoporosis threshold, bisphosphonate contraindications, denosumab side effects rebound fractures, osteoporosis prevention diet exercise ---
Browse by Medical Category
Explore content organized by medical specialties and systems