Clinical videos + HTML notes for NEET PG-ready revision.
Streamora lets you upload case-based videos, attach rich HTML notes, like and comment on other clinicians’ posts, follow creators and save structured exam-oriented pearls – all mobile-first and SEO-ready.
Why Streamora stands out for NEET PG aspirants: Unlike generic apps, we focus on high-yield topics like labour stages (from first to fourth, with management pitfalls), Rh-negative pregnancies (anti-D prophylaxis timing), and anatomy pearls (e.g., sacral hiatus for caudal blocks). Our community-driven notes include real residency cases—e.g., "Missed Rh isoimmunization leading to hydrops fetalis"—with attached flowcharts and MCQ-style tags for quick revision. Free, ad-light, and built by med students for med students.
Latest Medical Posts
High-yield medical discussions, NEET PG-flavoured notes and short clinical cases from all users.
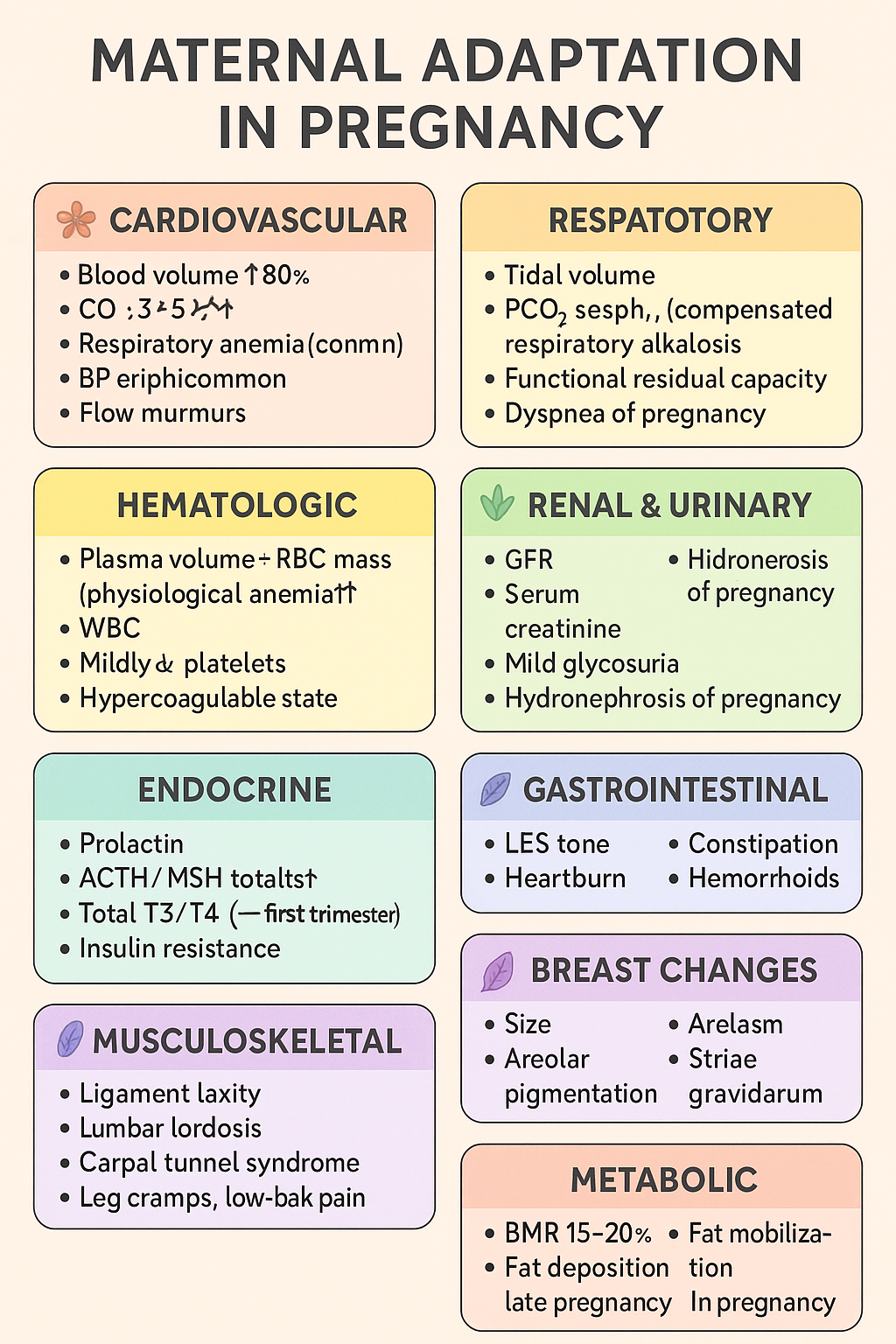
Maternal Adaptations in Pregnancy: Cardiovascular, Respiratory, Renal, Endocrine & Hematologic Changes | Complete Obstetrics Guide 2025
Below is your **complete, crisp but exhaustive stylish note** on **MATERNAL ADAPTATION IN PREGNANCY** — perfect for **NEET PG / INI-CET** and LWT article publishing. Presented in **high-yield, section-boxed format**. --- # ⭐ **MATERNAL ADAPTATIONS IN PREGNANCY — COMPLETE STYLISH NOTE (2025)** Pregnancy induces **multi-system physiologic adaptations** to support fetal growth, prepare for labor, and protect the mother from hemodynamic stresses. --- ## 🌸 **1. Cardiovascular Adaptations** ### 🔹 *Changes* * **Blood volume ↑ 40–50%** (plasma ↑ > RBC mass ↑ → *physiological anemia*). * **CO ↑ 30–50%** → peaks at 20–24 weeks. * **HR ↑ 10–20 bpm**. * **Systemic vascular resistance ↓** (progesterone-mediated vasodilation). * **BP ↓ in 2nd trimester**, returns to baseline in 3rd. * **Peripheral edema common** due to venous compression by gravid uterus. * **Flow murmurs, S3 may appear**. ### 🔹 *Clinical significance* * ↑ preload → protects from blood loss during delivery. * Supine position → **supine hypotension syndrome** (IVC compression). * Murmurs usually benign; still evaluate if symptomatic. --- ## 🌸 **2. Respiratory Adaptations** ### 🔹 *Changes* * **Tidal volume ↑ 30–40%**, minute ventilation ↑. * **PCO₂ ↓ → respiratory alkalosis (compensated)**. * **Functional residual capacity ↓** (diaphragm elevation by 4 cm). * **Dyspnea of pregnancy common** (physiological). ### 🔹 *Clinical significance* * Low PCO₂ → facilitates **placental CO₂ transfer**. * Increased ventilation → improved oxygenation for fetus. --- ## 🌸 **3. Hematologic Adaptations** ### 🔹 *Changes* * **Plasma volume ↑ 50%**, **RBC mass ↑ 20–30%** → dilution → **Hb ↓ (physiologic anemia)**. * **WBC ↑** (can reach 12–16k). * **Platelets mildly ↓** (gestational thrombocytopenia). * **Hypercoagulable state** → fibrinogen ↑, clotting factors ↑. ### 🔹 *Clinical significance* * Protects from postpartum hemorrhage. * ↑ VTE risk — especially postpartum. --- ## 🌸 **4. Renal & Urinary Adaptations** ### 🔹 *Changes* * **GFR ↑ 40–50%** (starts early). * **Serum creatinine ↓ 0.4–0.6 mg/dL**. * **Mild glycosuria** common. * **Hydronephrosis of pregnancy** (right > left) due to progesterone + uterine compression. ### 🔹 *Clinical significance* * Minor proteinuria acceptable (<300 mg/day). * Avoid misinterpreting physiologic glycosuria as diabetes. --- ## 🌸 **5. Endocrine Adaptations** ### 🔹 *Pituitary* * **Prolactin ↑** 10-fold → lactation prep. * **ACTH & MSH ↑** → pigmentation changes. ### 🔹 *Thyroid* * **Estrogen ↑ TBG**, total T3/T4 ↑; **free T4 normal**. * **hCG weak TSH activity → TSH ↓** (first trimester). ### 🔹 *Pancreas* * Early pregnancy: **insulin sensitivity ↑**. * Late pregnancy: **insulin resistance ↑** (placental hormones: hPL, cortisol) → predisposes to **GDM**. --- ## 🌸 **6. Gastrointestinal Adaptations** ### 🔹 *Changes* * **Progesterone ↓ LES tone** → heartburn. * **Gastric emptying ↓** → nausea/vomiting. * **Constipation** from prolonged transit time. * **Hemorrhoids** due to venous congestion. ### 🔹 *Clinical significance* * Morning sickness peaks at 9–10 weeks. * Hyperemesis gravidarum requires electrolyte correction. --- ## 🌸 **7. Musculoskeletal Adaptations** ### 🔹 *Changes* * **Relaxin + progesterone → ligament laxity**. * **Lumbar lordosis ↑** due to uterine weight. * **Carpal tunnel syndrome** possible. * **Leg cramps**, **low-back pain** common. ### 🔹 *Clinical significance* * Risk of falls increases. * Proper posture + exercises advised. --- ## 🌸 **8. Breast Changes** * **Size ↑**, ducts proliferate. * **Areolar pigmentation**, Montgomery tubercles prominent. * **Colostrum secretion** by late pregnancy. --- ## 🌸 **9. Dermatologic Adaptations** * **Linea nigra**, **melasma**, **striae gravidarum**. * **Spider angiomas**, palmar erythema (estrogen related). --- ## 🌸 **10. Metabolic Adaptations** * **Basal metabolic rate ↑ 15–20%**. * **Fat deposition ↑** early pregnancy. * Late pregnancy: catabolic → **fat mobilization** for maternal energy, glucose spared for fetus. --- # ⭐ **ULTRA-SHORT MEMORY HACK TABLE** | System | Key Adaptation | Why it Happens | | --------------- | ---------------------- | ---------------------------------------------------- | | CVS | CO ↑ 50%, plasma ↑ 50% | To meet fetal perfusion & buffer delivery blood loss | | Respiratory | TV ↑, PCO₂ ↓ | Better fetal CO₂ removal | | Renal | GFR ↑ 50% | Remove maternal/fetal waste | | Hematologic | Hypercoagulable | Prevent PPH | | Endocrine | Insulin resistance | Ensure fetal glucose | | GI | ↓ Motility | Progesterone effect | | Musculoskeletal | Ligament laxity | Prepare pelvis for birth | --- If you want, I can generate: ✅ **HTML-CSS-JS formatted article** (like your LWT posts) ✅ **MCQs (20/25/30 hard case-based)** ✅ **SEO title + description + keywords** ✅ **Custom medical diagram for maternal adaptations** Just tell me **which output you want next**.
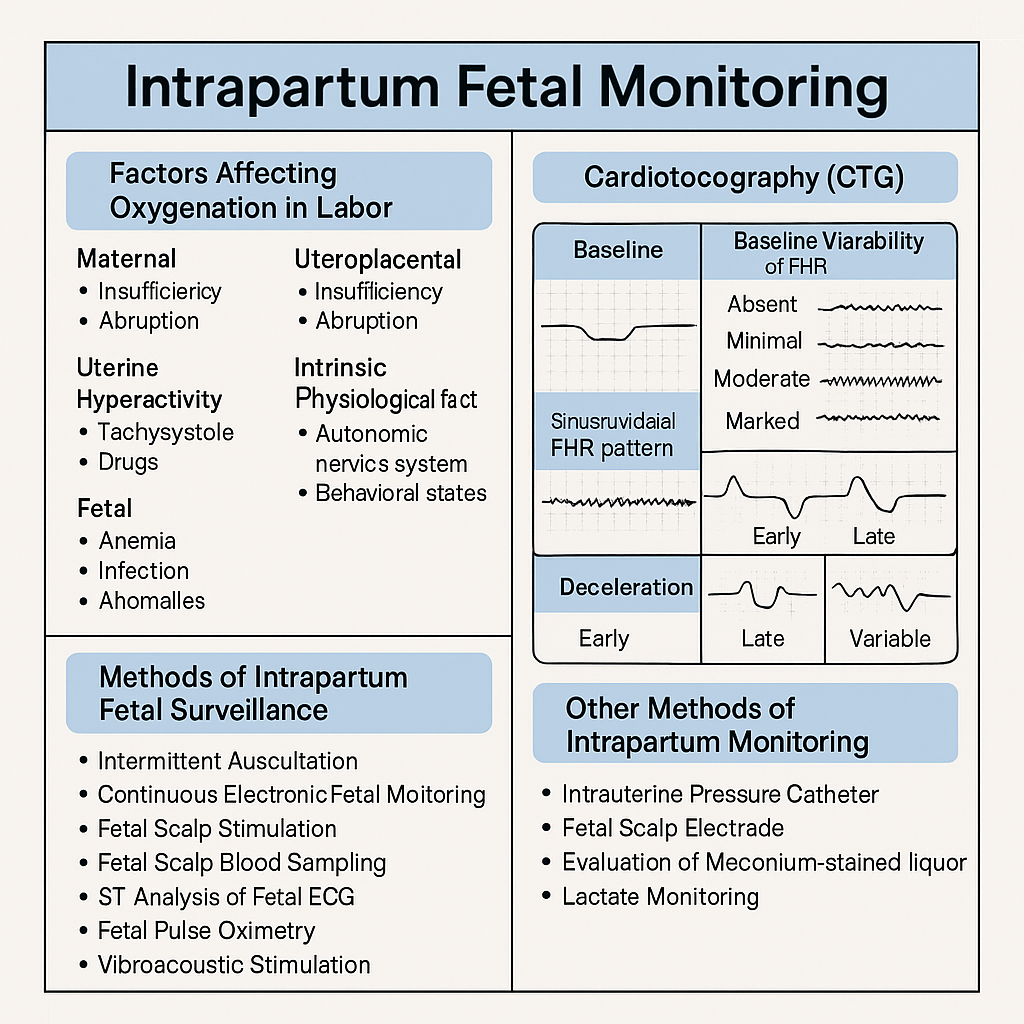
Intrapartum Fetal Monitoring: CTG Interpretation, Decelerations, Sinusoidal Pattern & Complete Management Guide 2025
Below are **30 detailed intrapartum fetal monitoring case scenarios with complete management**, written in **NEET PG / INI-CET exam style**. Each scenario includes **clinical context → CTG finding → diagnosis → step-wise management**. --- # ✅ **30 CASE SCENARIOS WITH DETAILED MANAGEMENT (Intrapartum Fetal Monitoring)** --- ## **1️⃣ Case — Late Decelerations in a Preeclamptic Mother** A 25-year-old primigravida, 4 cm dilated, on oxytocin. CTG shows **recurrent late decelerations**, baseline 150, variability <5 bpm. ### **Diagnosis** Uteroplacental insufficiency from **preeclampsia + hyperstimulation**. ### **Management** 1. Stop oxytocin 2. Left lateral position 3. IV fluids 4. If contraction frequency >5/10 min → **tocolysis (terbutaline 0.25 mg SC)** 5. If no improvement → **FBS** 6. If pH <7.20 or tracing deteriorates → **Emergency LSCS** --- ## **2️⃣ Case — Variable Decelerations with Oligohydramnios** G2P1, term labor, CTG shows **variable decelerations with shoulders**, adequate variability. ### **Diagnosis** Cord compression due to oligohydramnios. ### **Management** 1. Maternal repositioning 2. Amnioinfusion 3. Continue labor if variability normal 4. If severe recurrent variables + loss of variability → expedite delivery --- ## **3️⃣ Case — Sinusoidal Pattern** Rh-negative woman, fetus 38 weeks. CTG: **true sinusoidal pattern**. ### **Diagnosis** Severe fetal anemia. ### **Management** 1. Immediate evaluation (Kleihauer test, ultrasound MCA Doppler if time permits) 2. **Emergency LSCS** 3. Prepare NICU for transfusion --- ## **4️⃣ Case — Prolonged Deceleration from Cord Prolapse** During vaginal exam, a loop of cord felt. CTG shows **bradycardia at 80 bpm** for 4 minutes. ### **Management** 1. Lift presenting part manually 2. Knee–chest position 3. Call for emergency LSCS 4. Warm sterile saline-soaked gauze to prevent vasospasm 5. Deliver within **<30 minutes** --- ## **5️⃣ Case — Tachysystole-Induced Late Decelerations** Oxytocin infusion running, contractions 6/10 min. CTG: recurrent late decels. ### **Management** 1. Stop oxytocin immediately 2. Terbutaline 0.25 mg SC 3. Lateral position 4. Reassess 5. If persists → expedite delivery --- ## **6️⃣ Case — Minimal Variability for 50 Minutes** Primigravida in active labor. CTG: baseline 140, variability <5 bpm for 50 min, no decels. ### **Diagnosis** Non-reassuring CTG, possibly fetal sleep or medication effect. ### **Management** 1. Scalp stimulation 2. If acceleration present → reassuring 3. If absent → FBS or continuous monitoring 4. Continue labor if other parameters normal --- ## **7️⃣ Case — Meconium-Stained Liquor with Abnormal CTG** Thick meconium + variable decels + reduced variability. ### **Management** 1. Intrauterine resuscitation 2. Amnioinfusion (if available) 3. Prepare for operative delivery 4. NICU standby for Meconium Aspiration Syndrome --- ## **8️⃣ Case — Prolonged Deceleration After Epidural** Immediately after epidural, FHR drops to 90 bpm for 3 minutes. ### **Diagnosis** Maternal hypotension causing decreased uteroplacental flow. ### **Management** 1. Left lateral position 2. IV fluid bolus 3. Vasopressor (phenylephrine preferred) 4. If persists beyond 5 minutes → consider LSCS --- ## **9️⃣ Case — Fetal Tachycardia with Maternal Fever** CTG shows FHR 180 bpm, moderate variability; maternal temp 101°F. ### **Diagnosis** Chorioamnionitis. ### **Management** 1. Broad-spectrum antibiotics 2. Acetaminophen 3. Expedite delivery (not LSCS solely for fever) 4. Avoid prolonged labor --- ## **🔟 Case — Arrest of Descent + Late Decelerations** Second stage, fully dilated, prolonged pushing, late decels appear. ### **Management** 1. Check for instrumental eligibility 2. **Forceps or vacuum** if head low 3. If not eligible → emergency LSCS --- ## **1️⃣1️⃣ Case — Recurrent Severe Variable Decelerations** CTG: variable decels dropping to 70 bpm for 60–90 sec. ### **Management** 1. Lateral positioning 2. Amnioinfusion 3. Reduce contractions if tachysystole 4. If persistent → operative delivery --- ## **1️⃣2️⃣ Case — Fetal Scalp pH Borderline** FBS pH = 7.22. ### **Management** 1. Correct reversible causes 2. Repeat FBS in 30 min 3. If worsens → expedite delivery --- ## **1️⃣3️⃣ Case — Loss of Variability with Bradycardia** Baseline 90 bpm, absent variability. ### **Diagnosis** Advanced fetal hypoxia. ### **Management** 1. Immediate decision for LSCS 2. No role of waiting or FBS --- ## **1️⃣4️⃣ Case — CTG Unable to Trace Due to Obesity** During labor, external CTG poor quality. ### **Management** 1. Switch to **fetal scalp electrode (FSE)** 2. Use IUPC for contraction monitoring 3. Continue labor normally if FHR normal --- ## **1️⃣5️⃣ Case — Category III CTG in Trial of Labor After Cesarean (TOLAC)** Late decels + minimal variability + scar tenderness. ### **Diagnosis** Scar rupture suspected. ### **Management** 1. Immediate emergency LSCS 2. Do NOT attempt instrumental delivery --- ## **1️⃣6️⃣ Case — Hyperstimulation Causing Decelerations** Misoprostol induction; CTG shows tachysystole + decels. ### **Management** 1. Stop prostaglandin 2. Tocolysis 3. Continuous monitoring 4. If fetal distress → emergency delivery --- ## **1️⃣7️⃣ Case — True Sinusoidal Pattern from Fetomaternal Hemorrhage** CTG sinusoidal; Kleihauer test positive. ### **Management** 1. Emergency delivery 2. Neonatal transfusion preparation --- ## **1️⃣8️⃣ Case — Prolonged Decel During Second Stage** Mother pushing vigorously; CTG shows bradycardia. ### **Management** 1. Stop pushing 2. Reassess for instrument delivery 3. If head + station → vacuum/forceps 4. Otherwise → LSCS --- ## **1️⃣9️⃣ Case — Mild Variable Decelerations with Normal Variability** Intermittent variables, contraction-associated. ### **Management** 1. Reassurance 2. Continue monitoring No intervention required. --- ## **2️⃣0️⃣ Case — Shoulder Dystocia + Bradycardia** Delivery nearly complete, FHR falls to 70 bpm. ### **Management** 1. McRoberts + suprapubic pressure 2. Deliver shoulders quickly 3. Neonatal resuscitation readiness --- ## **2️⃣1️⃣ Case — Cord Around Neck Detected on Ultrasound Before Labor** During labor → variable decels appear. ### **Management** 1. Continue monitoring 2. If severe or persistent → expedite delivery 3. Do not intervene solely for nuchal cord --- ## **2️⃣2️⃣ Case — Prolapsed Cord in Breech** CTG severe bradycardia. ### **Management** 1. Knee–chest position 2. Manual elevation of presenting part 3. Emergency LSCS --- ## **2️⃣3️⃣ Case — Minimal Variability from Opioid Analgesia** Given pethidine 15 min ago; variability <5. ### **Management** 1. Observe for 30–60 min 2. If variability recovers → continue 3. If not → evaluate for fetal hypoxia --- ## **2️⃣4️⃣ Case — Reassuring CTG in Low-Risk Labor** Baseline 140, variability 10, accelerations present. ### **Management** Continue routine monitoring. --- ## **2️⃣5️⃣ Case — Excessive Maternal Dehydration** CTG shows fetal tachycardia 170 bpm. ### **Management** 1. IV fluid bolus 2. Assess maternal vitals 3. Continue monitoring --- ## **2️⃣6️⃣ Case — Placental Abruption Suspected** Pain + bleeding + fetal tachycardia → later bradycardia. ### **Management** 1. Stabilize mother 2. Immediate LSCS if fetus alive 3. Vaginal delivery only if imminent --- ## **2️⃣7️⃣ Case — IUGR Baby with Recurrent Late Decelerations** CTG: late decels + reduced variability. ### **Management** 1. Intrauterine resuscitation 2. No role for prolonged labor 3. **Expedite delivery** --- ## **2️⃣8️⃣ Case — Maternal Seizure (Eclampsia)** CTG: prolonged decel. ### **Management** 1. Stabilize mother (MgSO₄, airway) 2. Left lateral position 3. If fetal recovery absent → LSCS --- ## **2️⃣9️⃣ Case — Vaginal Birth After Multiple Variables** CTG mostly reassuring except mild variables. ### **Management** 1. Continue monitoring 2. Check for cord issues 3. No intervention unless severe --- ## **3️⃣0️⃣ Case — Failure of Fetal Response to Scalp Stimulation** Minimal variability, no acceleration after stimulation. ### **Diagnosis** Hypoxia suspected. ### **Management** 1. FBS if available 2. If pH abnormal → immediate delivery 3. If not available → treat as pathological CTG → expedite delivery --- If you want, I can also produce: ✅ **HTML + CSS + JS EXAM MODE MCQs (25/30/50)** ✅ **SEO title/description/keywords** ✅ **A medical diagram image for intrapartum fetal monitoring** Just say **“generate MCQs”**, **“generate image”**, or **“give SEO”**. Below is your **complete, concise-but-exhaustive master reference** on **Intrapartum Fetal Monitoring** — fully aligned with NEET PG / INI-CET high-yield requirements. --- # ⭐ **INTRAPARTUM FETAL MONITORING — COMPLETE DETAILED NOTES (2025)** --- ## **1️⃣ Factors Affecting Fetal Oxygenation During Labor** Fetal oxygenation depends on uninterrupted flow across **four levels**: ### **A. Maternal Factors** * **Maternal oxygenation:** Hypoxia, severe anemia, pulmonary disease. * **Uterine perfusion:** Hypotension (epidural, hemorrhage), dehydration, aortocaval compression. * **Uterine hyperactivity:** Tachysystole (>5 contractions/10 min), hypertonus ↓ intervillous blood flow. * **Drugs:** β-agonists ↑ fetal tachycardia; opioids ↓ variability. ### **B. Uteroplacental Factors** * Placental insufficiency (hypertension, preeclampsia, post-maturity). * Placental abruption, infarction, previa, accreta spectrum. * Umbilical cord compression (oligohydramnios, cord prolapse, tight nuchal cord). ### **C. Fetal Factors** * Fetal anemia, infections, acidosis. * Congenital anomalies (especially CNS, cardiac). * Prematurity → reduced variability. ### **D. Intrinsic Physiological Factors** * Autonomic nervous system balance (sympathetic/parasympathetic). * Fetal behavioral states (quiet sleep cycles ↓ variability). --- ## **2️⃣ Methods of Intrapartum Fetal Surveillance** ### **A. Intermittent Auscultation (IA)** * Using **Pinard stethoscope** or **Doppler**. * Low-risk pregnancies. * Frequency: * **1st stage:** every 30 min * **2nd stage:** every 5 min * Look for: baseline, accelerations, decelerations. ### **B. Continuous Electronic Fetal Monitoring (EFM / CTG)** * External US transducer + tocodynamometer. * Internal scaling: scalp electrode + IUPC (intrauterine pressure catheter) when needed. ### **C. Fetal Scalp Stimulation** * Acceleration after stimulation → reassuring (pH > 7.2). ### **D. Fetal Scalp Blood Sampling (FBS)** → Direct measure of fetal acid-base status. * **Normal pH ≥ 7.25** * **Borderline 7.21–7.24** * **Abnormal < 7.20** → urgent delivery. ### **E. ST-Analysis of Fetal ECG (STAN)** * Detects myocardial hypoxia (ST changes). * Used with CTG. ### **F. Fetal Pulse Oximetry (rare)** * Reassurance if SpO₂ > 30%. ### **G. Vibroacoustic Stimulation** * Sound stimulus → acceleration = good oxygenation. --- ## **3️⃣ Cardiotocography (CTG) – Complete Interpretation** CTG has **5 components**: **Baseline, Variability, Accelerations, Decelerations, Contractions.** --- ## **3.1 Baseline Fetal Heart Rate** Normal: **110–160 bpm** ### **Tachycardia (>160 bpm) causes:** * Maternal fever (chorioamnionitis) * Fetal hypoxia early * Fetal anemia * Drugs: β-agonists, atropine ### **Bradycardia (<110 bpm) causes:** * Vagal stimulation (head compression) * Cord compression * Prolonged deceleration → late sign of hypoxia --- ## **3.2 Baseline Variability (BV)** Reflects fetal autonomic integrity. | **Type** | **Range** | **Significance** | | --------------------- | ------------ | ------------------------------------------ | | Absent | 0 bpm | Severe hypoxia, acidosis, drugs | | Minimal | <5 bpm | Sleep cycle, opioids, prematurity, hypoxia | | **Moderate (Normal)** | **6–25 bpm** | Good oxygenation | | Marked | >25 bpm | Early hypoxia, cord compression | --- ## **3.3 Accelerations** * Abrupt ↑ in FHR by ≥15 bpm for ≥15 sec. * **Reassuring sign** → fetal well-being. --- ## **3.4 Decelerations — Types & Complete Interpretation** ### **A. Early Decelerations** * Mirror contractions. * Due to **head compression**. * **Benign, no treatment.** ### **B. Late Decelerations** * Begin after the contraction peak → return after contraction ends. * Due to **uteroplacental insufficiency**. * **Always concerning**, esp. with absent variability. ### **C. Variable Decelerations** * Abrupt fall in FHR, variable shape. * Due to **cord compression**. * May have "shoulders" (pre- & post-acceleration). * Severe if >60 bpm drop lasting >60 sec. ### **D. Prolonged Deceleration** * FHR drop ≥15 bpm lasting **2–10 min**. * > 10 min = change in baseline. ### **E. Sinusoidal Pattern (MOST IMPORTANT)** **True Sinusoidal Pattern** * Smooth, regular, sine-wave oscillation (3–5 cycles/min) * Amplitude 5–15 bpm * No variability, no accelerations * **Causes:** * Severe fetal anemia (Rh isoimmunization, fetomaternal hemorrhage) * Twin-to-twin transfusion * Hypoxia late stage * **Immediate delivery required** **Pseudo-sinusoidal:** * Seen with opioids — benign. --- ## **4️⃣ NICE 2024 Categories of CTG Interpretation** | Category | Findings | Action | | ------------------------------- | -------------------------------------------------------- | ------------------------------------------------ | | **Normal (Category I)** | Baseline 110–160, Variability 6–25, No repetitive decels | Continue | | **Suspicious (Category II)** | One non-reassuring feature | Correct reversible causes, close monitoring | | **Pathological (Category III)** | ≥1 abnormal feature OR ≥2 non-reassuring | Immediate evaluation, FBS, or expedited delivery | ### **Features** **Reassuring:** * Baseline 110–160 * Variability 6–25 * No decelerations / early decels * Accelerations present **Non-reassuring:** * Baseline 100–109 or 161–180 * Variability <5 for 40–90 min * Variable decels with features * Single prolonged decel <3 min **Abnormal:** * Baseline <100 or >180 * Variability <5 for >90 min * Late decels / prolonged decels >3 min * Sinusoidal pattern --- ## **5️⃣ Management of Abnormal CTG** ### **A. Correct Reversible Causes** * Left lateral position * IV fluids → treat maternal hypotension * Stop oxytocin (if tachysystole) * Tocolysis if uterine hyperstimulation (Terbutaline 0.25 mg SC) * Oxygen (only if maternal hypoxia) ### **B. Fetal Assessment** * Fetal scalp stimulation * FBS (pH or lactate) ### **C. Delivery** * If pH <7.20 OR pathological CTG persists * Emergency LSCS or instrumental delivery depending on stage --- ## **6️⃣ Other Methods of Intrapartum Monitoring** ### **A. Intrauterine Pressure Catheter (IUPC)** * Measures **Montevideo units** * Adequate labor: **>200 MVU** ### **B. Fetal Scalp Electrode (FSE)** * Accurate beat-to-beat FHR * Used when external CTG is poor. ### **C. Meconium-stained liquor evaluation** * Thick meconium + abnormal CTG → intrapartum hypoxia risk. ### **D. Lactate Monitoring** * Fetal scalp lactate <4.8 mmol/L reassuring. --- ## **7️⃣ Quick High-Yield Revision Table** | Topic | Key Points | | ------------------------------- | ------------------------------- | | Best indicator of fetal hypoxia | **Reduced variability** | | Worst CTG sign | **Sinusoidal pattern** | | Earliest sign of hypoxia | **Tachycardia** | | Most common deceleration | **Variable (cord compression)** | --- If you want, I can also generate: ✅ SEO title, description & keywords ✅ 25 hard case-based MCQs (HTML + CSS + JS EXAM MODE) ✅ 25 case scenarios with management ✅ Medical diagram image (via image generator) Just tell me **“continue”** with what you need.
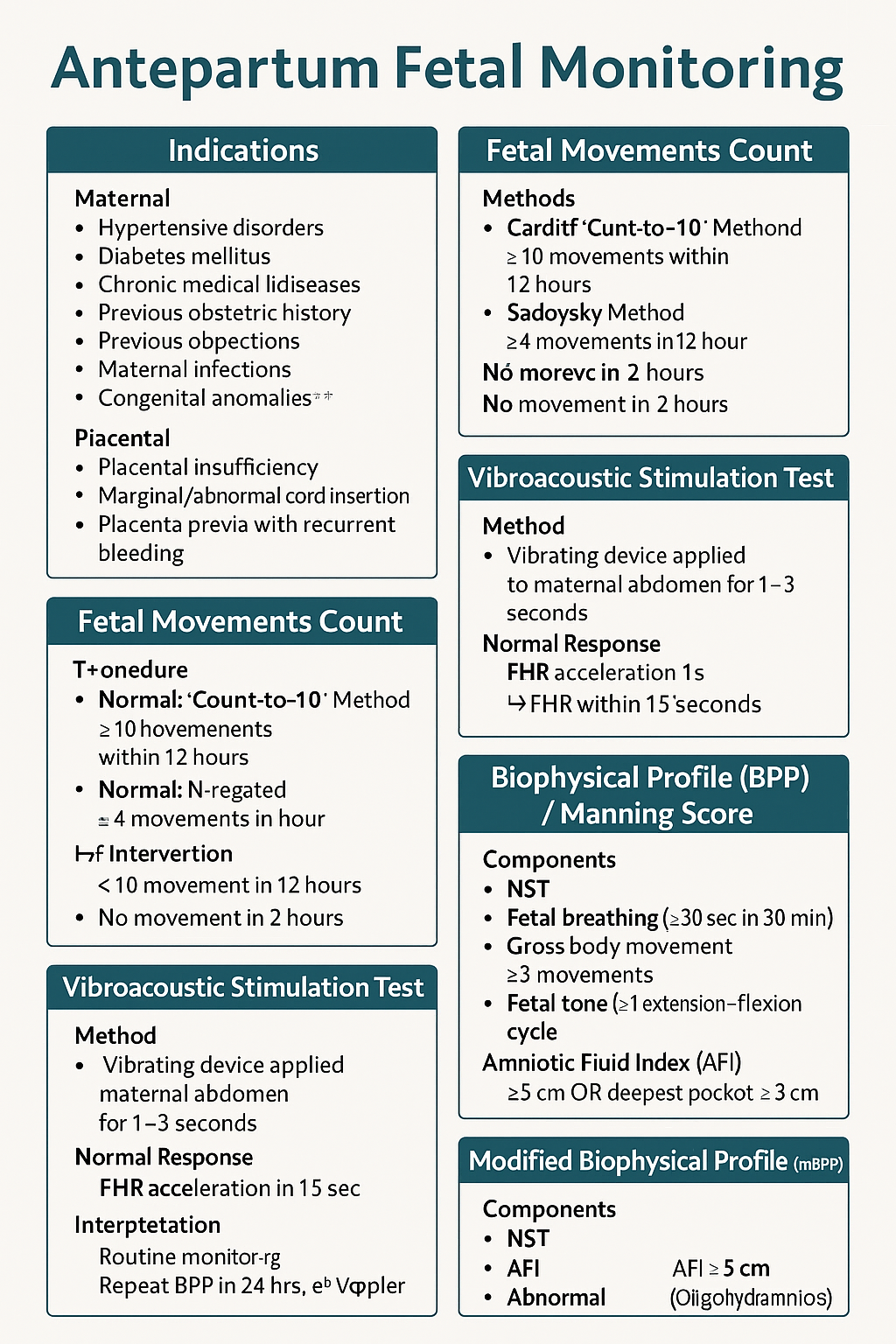
Antepartum Fetal Monitoring: Indications, NST, Biophysical Profile, Modified BPP & Vibroacoustic Test | Complete Obstetrics Guide 2025
--- # ⭐ **ANTEPARTUM FETAL MONITORING — COMPLETE HIGH-YIELD REFERENCE (NEET PG / INI-CET)** Antepartum fetal surveillance aims to detect **early fetal hypoxia** to prevent stillbirth, reduce perinatal morbidity, and guide timing of delivery. It assesses **placental function**, **oxygenation**, **neurological integrity**, and **fetal compensatory mechanisms**. --- # **1️⃣ Indications for Antepartum Fetal Monitoring** ### **A. Maternal Indications** * **Hypertensive disorders:** Gestational HTN, preeclampsia, eclampsia * **Diabetes mellitus:** GDM requiring insulin/OADs, pre-gestational DM * **Chronic medical diseases:** * Chronic hypertension * Renal disease * Autoimmune disease (SLE, APLA syndrome) * Cardiac disease * Thyroid disease with complications * **Previous obstetric history:** * Previous stillbirth * Previous IUGR baby * Previous neonatal death * Isoimmunization/Rh alloimmunization * **Maternal infections:** TORCH with fetal involvement * **Advanced maternal age (>35)** * **Post-dated pregnancy (>40 weeks)** ### **B. Fetal Indications** * **Decreased fetal movements** * **IUGR (Symmetric/Asymmetric)** * **Oligohydramnios / Polyhydramnios** * **Multiple pregnancy with complications** * **Fetal anemia / hydrops** * **Congenital anomalies** ### **C. Placental Indications** * Placental insufficiency * Marginal/Abnormal cord insertion * Placenta previa with recurrent bleeding --- # **2️⃣ Fetal Movement Count (FMC / Kick Count)** Fetal movements reflect fetal well-being (neurological + metabolic status). ### **Methods** ### **A. Cardiff Count-to-10 Method** * Mother records movements daily. * **Normal:** 10 movements within 12 hours. ### **B. Sadovsky Method** * Count movements for 1 hour after meals. * **Normal:** ≥4 movements/hour. ### **When to worry?** * **<10 movements in 12 hours** * **<4 movements in 1 hour** * **No movement in 2 hours** → urgent evaluation (NST/BPP) ### **Management of Decreased Fetal Movements** 1. Immediate **NST** 2. If NST non-reactive → **BPP** 3. If BPP equivocal → **Doppler studies** 4. If evidence of fetal compromise → **Delivery based on GA** --- # **3️⃣ Non-Stress Test (NST)** NST measures **fetal heart rate accelerations** in response to fetal movements via cardiotocography. ### **Procedure** * Done after **28–32 weeks** (mature autonomic nervous system). * Duration: **20 minutes** (extend to 40 minutes if needed). --- ## **Interpretation (Reactive vs Non-Reactive)** ### ✔ **Reactive NST (Normal)** * **≥2 accelerations** in 20 minutes * Acceleration criteria: * **≥15 bpm for ≥15 sec** (≥32 weeks) * **≥10 bpm for ≥10 sec** (<32 weeks) ### ✔ **Non-Reactive NST** * <2 accelerations in 40 minutes * Suggests fetal sleep cycle, hypoxia, CNS depression. ### **Causes of Non-Reactive NST** * Fetal sleep * Maternal drug intake (MgSO₄, opioids, sedatives) * Hypoxia * Prematurity * Congenital anomalies ### **Next Steps in Non-Reactive NST** * Vibroacoustic stimulation test * BPP * Contraction stress test (rarely used today) * Doppler studies --- # **4️⃣ Vibroacoustic Stimulation Test (VAST)** Used to differentiate fetal sleep from hypoxia in non-reactive NST. ### **Method** * A vibrating device (artificial larynx) applied to maternal abdomen for **1–3 seconds**. ### **Normal Response** * FHR acceleration within **15 seconds** * Converts non-reactive NST → **reactive** ### **Significance** * High negative predictive value * Reduces need for BPP --- # **5️⃣ Biophysical Profile (BPP) / Manning Score** Combines **NST + ultrasound parameters** assessing fetal CNS integrity + oxygenation. ### **Components (Total 10 points)** Each gets **2 = normal**, **0 = abnormal** | Component | Normal Criteria (2 points) | | ------------------------------ | --------------------------------- | | **NST** | Reactive | | **Fetal breathing** | ≥30 sec in 30 min | | **Gross body movement** | ≥3 movements | | **Fetal tone** | ≥1 extension–flexion cycle | | **Amniotic Fluid Index (AFI)** | AFI ≥5 cm OR deepest pocket ≥2 cm | --- ## **Scoring & Interpretation** | Score | Interpretation | Management | | -------- | -------------- | ------------------------------------------- | | **8–10** | Normal | Routine monitoring | | **6** | Equivocal | Repeat BPP in 24 hrs; evaluate Doppler | | **4** | Abnormal | Risk of fetal hypoxia → Delivery if ≥34 wks | | **0–2** | Severe hypoxia | Immediate delivery | --- # **6️⃣ Modified Biophysical Profile (mBPP)** Simplified & widely used. ### **Components** 1. **NST** 2. **AFI (Amniotic Fluid Index)** ### **Interpretation** * **Normal:** Reactive NST + AFI ≥5 cm * **Abnormal:** * Non-reactive NST * AFI <5 cm (Oligohydramnios) → placental insufficiency ### **Management** * If abnormal mBPP → full BPP or Doppler; consider delivery based on GA. --- # **7️⃣ Contraction Stress Test (OBSOLETE mostly)** Assesses fetal response to **uterine contractions** → risk of late decelerations. Rarely done due to risk + availability of Doppler and BPP. --- # **8️⃣ Putting It All Together — Management Algorithm** ### **Decreased fetal movements →** 1. **NST** 2. If reactive → reassure 3. If non-reactive → repeat + VAST 4. If still non-reactive → BPP 5. * **BPP ≤4** → Delivery * **BPP 6** → Repeat in 24 hrs * **BPP 8–10** → Continue routine follow-ups 6. Assess **AFI, Doppler, maternal condition** --- # **9️⃣ Important Clinical Correlations** ### **NST becomes abnormal earliest in fetal hypoxia** CNS activity reduces → loss of accelerations. ### **BPP components lost in sequence during hypoxia (Late → Early loss)** 1. **NST** 2. **Fetal breathing** 3. **Gross movement** 4. **Fetal tone** (last to disappear) 5. **AFI reduced** from chronic utero-placental insufficiency ### **AFI is chronic marker**; NST is acute marker. --- # ⭐ **HIGH-YIELD VALUES (MUST REVISE)** * Reactive NST: **≥2 accelerations** (15 × 15) * Tone: 1 flexion–extension * Breathing: ≥1 episode ≥30 sec * Movement: ≥3 body movements * AFI: Normal ≥5 cm * Modified BPP = NST + AFI * Sleep cycle: **20–40 min** → extend NST to 40 min --- --- # ⭐ **25 CASE SCENARIOS WITH DETAILED MANAGEMENT** *(Antepartum Fetal Surveillance: FMC, NST, BPP, VAST, mBPP)* --- # **1️⃣ Case Scenario – Decreased Fetal Movements at 34 Weeks** A 28-year-old G2P1 at 34 weeks reports **no fetal movements for 8 hours**. ### **Management** 1. Immediate **NST** 2. If **reactive** → reassure, daily kick count 3. If **non-reactive** → extend to 40 min 4. If still non-reactive → **VAST** 5. If remains non-reactive → **BPP** 6. * **BPP ≥8** → Follow-up * **BPP ≤4** → Deliver based on GA --- # **2️⃣ Case Scenario – Non-Reactive NST in a Diabetic Mother** GDM on insulin at 36 weeks undergoes NST → **non-reactive** after 40 minutes. ### **Management** 1. Perform **VAST** 2. If reactive → repeat NST in 1 week 3. If still non-reactive → **Full BPP** 4. If BPP score **≤4** → Plan delivery 5. Assess **AFI & Doppler** for placental insufficiency --- # **3️⃣ Case Scenario – Oligohydramnios with IUGR** 30-year-old at 32 weeks with **AFI = 4 cm**, EFW <10th percentile. ### **Management** 1. Start **modified BPP (NST + AFI)** 2. Daily NST 3. Doppler: **Umbilical artery S/D ratio** 4. If AEDF/REDF → **Immediate delivery** 5. If NST non-reactive → full BPP 6. Steroids if <34 weeks --- # **4️⃣ Case – Post-Dated Pregnancy (41 Weeks)** Patient at 41+2 weeks shows decreased fetal movement. ### **Management** 1. **NST + AFI** 2. If NST reactive & AFI normal → induce labour within 24–48 hrs 3. If NST non-reactive → BPP 4. BPP ≤6 → Deliver 5. Continuous intrapartum monitoring --- # **5️⃣ Case – Preeclampsia with Severe Features** 32 weeks, BP 160/110, proteinuria +++, fetus active. ### **Management** 1. Daily **NST** 2. Twice-weekly **BPP** 3. Doppler (UA + MCA) weekly 4. Magnesium sulfate for seizure prophylaxis 5. Deliver at 34 weeks or earlier if fetal compromise --- # **6️⃣ Case – Chronic Hypertension with Reduced Movements** 35-year-old with chronic HTN reports <4 kicks in 1 hr. ### **Management** 1. Immediate **NST** 2. If non-reactive → BPP 3. If AFI <5 → suspect placental insufficiency 4. Admit, daily surveillance 5. Deliver if BPP ≤4 or Doppler abnormal --- # **7️⃣ Case – IUGR with Normal NST** 29 weeks, IUGR but **reactive NST**. ### **Management** 1. Continue **twice-weekly NST** 2. Weekly Doppler (UA/ MCA/ CPR ratio) 3. Growth scan every 2 weeks 4. Deliver if Doppler deteriorates or NST becomes abnormal --- # **8️⃣ Case – Polyhydramnios with GDM** 30-year-old with polyhydramnios, NST reactive. ### **Management** 1. Twice-weekly NST 2. AFI monitoring 3. Doppler weekly 4. Induce at 38–39 weeks 5. Prepare for shoulder dystocia risk --- # **9️⃣ Case – Decreased Fetal Movement in Obese Mother** NST shows **baseline variability minimal**. ### **Management** 1. Rule out maternal meds, sleep cycle 2. Extend NST + VAST 3. If still abnormal → BPP 4. Deliver if BPP ≤4 --- # **🔟 Case – Rh-Isoimmunization** 28 weeks, MCA PSV >1.5 MOM (fetal anemia suspected). ### **Management** 1. Immediate **NST** 2. If non-reactive → BPP 3. Plan **intrauterine transfusion** 4. After IUT: Daily NST --- # **1️⃣1️⃣ Case – Twin Pregnancy with Growth Discordance** NST non-reactive for smaller twin. ### **Management** 1. VAST 2. If still non-reactive → BPP for each twin 3. Doppler UA/MCA/ Ductus venosus 4. Deliver if evidence of compromise --- # **1️⃣2️⃣ Case – Maternal Hypoglycemia Before NST** NST shows no accelerations. ### **Management** 1. Give oral glucose 2. Repeat NST 3. If becomes reactive → normal 4. If persistently non-reactive → VAST → BPP --- # **1️⃣3️⃣ Case – Placental Abruption Suspicion** Pain + bleeding + reduced movements. ### **Management** 1. **Immediate NST** 2. If late decelerations / bradycardia → **Immediate delivery** 3. Stabilize mother --- # **1️⃣4️⃣ Case – COVID Positive Mother with Decreased Movements** NST non-reactive. ### **Management** 1. Rule out maternal fever, hypoxia 2. Oxygen + hydration 3. VAST 4. If still non-reactive → BPP 5. Deliver if fetal compromise --- # **1️⃣5️⃣ Case – Smoking Mother with IUGR** NST shows decreased variability. ### **Management** 1. VAST 2. BPP 3. Doppler UA 4. Nicotine cessation + fetal surveillance every 2–3 days --- # **1️⃣6️⃣ Case – Absent Fetal Breathing on BPP** BPP = 6/10 (breathing absent). ### **Management** 1. Repeat BPP in 24 hrs 2. If repeat BPP ≤6 → Deliver 3. Continuous NST monitoring --- # **1️⃣7️⃣ Case – Low AFI but Reactive NST** AFI = 4 cm at 37 weeks. ### **Management** 1. Diagnose **oligohydramnios** 2. Admit, hydration 3. Modified BPP daily 4. Deliver at 37–38 weeks --- # **1️⃣8️⃣ Case – Maternal Seizure on MgSO₄** NST shows minimal variability (drug effect). ### **Management** 1. Continue monitoring 2. Do not interpret variability during MgSO₄ therapy 3. Use **BPP** instead of NST --- # **1️⃣9️⃣ Case – Poorly Controlled Diabetes** 36 weeks, polyhydramnios + macrosomia. ### **Management** 1. NST every 2–3 days 2. Weekly BPP 3. Deliver at 38 weeks 4. Prepare for shoulder dystocia --- # **2️⃣0️⃣ Case – Maternal Dehydration** NST non-reactive. ### **Management** 1. Give IV fluids 2. Repeat NST 3. If reactive → dehydration cause 4. If persists → BPP --- # **2️⃣1️⃣ Case – Postpartum Hemorrhage Risk Mother** Placenta previa major. ### **Management** 1. Weekly NST 2. BPP if NST abnormal 3. Plan elective C-section at 36–37 weeks --- # **2️⃣2️⃣ Case – Fetal Tachycardia** FHR 170 bpm in NST. ### **Management** 1. Exclude maternal fever, dehydration, drugs 2. Treat maternal cause 3. If persists → BPP + Doppler 4. Consider delivery if fetal compromise --- # **2️⃣3️⃣ Case – Mother on Sedatives** NST non-reactive. ### **Management** 1. Document medication effect 2. Perform BPP instead of repeating NST 3. Reassure if BPP normal --- # **2️⃣4️⃣ Case – Sudden IUD Suspicion** No FHR detected in NST. ### **Management** 1. Confirm with ultrasound 2. Evaluate cause (abruption, cord accident) 3. Manage according to GA and maternal stability --- # **2️⃣5️⃣ Case – Preterm (<32 Weeks) Non-Reactive NST** At 30 weeks, NST non-reactive. ### **Management** 1. Extend NST to 40 min 2. Apply VAST 3. If still non-reactive → BPP 4. If BPP ≤4 → Deliver after steroid cover 5. If BPP normal → prematurity likely cause ---
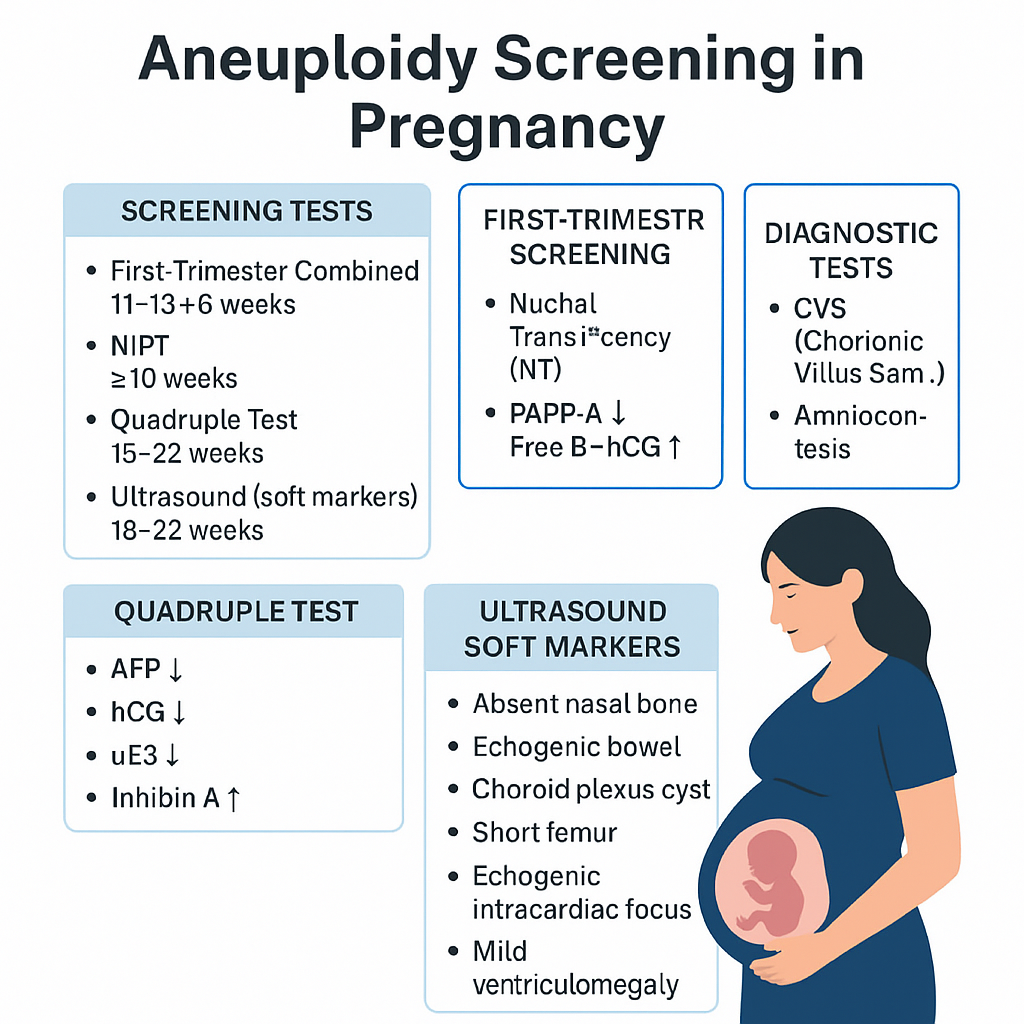
Aneuploidy Screening in Pregnancy: First Trimester, Quadruple Test, NIPT & Soft Markers | Complete Guide 2025
--- # ⭐ **Aneuploidy Screening in Pregnancy — Complete Obstetric Guide** Aneuploidy = **abnormal number of chromosomes** (most clinically relevant: **Trisomy 21, 18, 13**, Turner syndrome). Goal of screening = **identify pregnancies at increased risk** early enough to offer **diagnostic testing**. --- # **1. Why Aneuploidy Occurs (Basic Pathophysiology)** * **Meiotic nondisjunction** → failure of homologous chromosomes/sister chromatids to separate. * **Common in maternal meiosis I** (age-related). * **Trisomy 21 risk increases exponentially with maternal age**. * Mosaicism occurs if nondisjunction happens post-zygotically. --- # **2. High-Risk Factors** * Advanced maternal age (≥35 yrs). * Previous pregnancy with aneuploidy. * Parental balanced translocation (esp. Robertsonian). * Abnormal ultrasound markers (NT ↑, absent nasal bone, echogenic bowel, cardiac defects). * Abnormal biochemical screening results. --- # **3. Overview of Screening Timeline** | Gestation | Test | | ------------------- | ------------------------------------------------------------- | | **11–13+6 weeks** | First-trimester combined screening (NT + PAPP-A + free β-hCG) | | **10 weeks onward** | NIPT / cfDNA (highest accuracy) | | **15–22 weeks** | Second-trimester quadruple test | | **18–22 weeks** | Targeted anomaly scan (soft markers) | **Screening ≠ diagnosis.** Diagnostic tests = **CVS (10–13 wks)**, **Amniocentesis (≥15 wks)**, **FISH/karyotype/microarray**. --- # **4. First-Trimester Screening (11–13+6 Weeks)** ## **Components** 1. **Nuchal translucency (NT):** * Measured at CRL 45–84 mm * **NT >3.5 mm = major risk marker** * Increased NT → Trisomy 21/18/13, cardiac defects, Noonan syndrome, skeletal dysplasias 2. **Biochemical markers:** * **PAPP-A ↓**: Trisomy 21/18, placental insufficiency * **Free β-hCG ↑**: Trisomy 21 * **Free β-hCG ↓**: Trisomy 18/13 ## **Detection rate:** ~85–90% for T21 when combined. --- # **5. NIPT / cfDNA (Non-Invasive Prenatal Testing)** * Can be done **from 10 weeks onward**. * Analyzes **cell-free fetal DNA** in maternal blood. * **Most accurate screening test**. ## **Detects** * **Trisomy 21, 18, 13** * **Sex chromosome aneuploidies** (Turner, Klinefelter) * Microdeletions (low PPV, not recommended routinely) ## **Not diagnostic**, but: * **Sensitivity**: * T21 ≈ 99% * T18 ≈ 97–98% * T13 ≈ 92% ## **Causes of false results** * Confined placental mosaicism * Vanishing twin * Maternal malignancy * Low fetal fraction (<4%) --- # **6. Second-Trimester Quadruple Test (15–22 Weeks)** Markers: * **AFP** * **hCG** * **uE3 (unconjugated estriol)** * **Inhibin-A** ## **Patterns** ### **Trisomy 21** * **AFP ↓** * **uE3 ↓** * **hCG ↑** * **Inhibin-A ↑** ### **Trisomy 18** * **AFP ↓** * **uE3 ↓** * **hCG ↓** * **Inhibin-A normal** ### **Open neural tube defects** * **AFP ↑↑** Detection rate: * **~75% for T21** --- # **7. Ultrasound Soft Markers (18–22 Weeks)** ### **Major structural markers** * Cardiac defects (AV canal) → T21 * Holoprosencephaly → T13 * Omphalocele → T18 * Diaphragmatic hernia * Renal anomalies ### **Soft markers (non-structural)** | Marker | Association | | -------------------------------------- | --------------- | | **Absent nasal bone** | T21 | | **Echogenic intracardiac focus (EIF)** | Mild ↑ T21 risk | | **Echogenic bowel** | T21, CMV, CF | | **Short femur/humerus** | T21 | | **Choroid plexus cyst** | T18 | | **Single umbilical artery** | T18, T13 | | **Mild ventriculomegaly** | Aneuploidy risk | Soft markers **modify risk**, not diagnostic. --- # **8. Integrated & Sequential Screening** ### **Integrated test** * Combines first-trimester + second-trimester results * Highest combined detection before NIPT * Detection: **~94–95%**, but results available only in 2nd trimester ### **Sequential screening** * If first-trimester is high-risk → offer NIPT/CVS * If low-risk → continue with second trimester screening * More practical than integrated approach --- # **9. Diagnostic Tests (When Screening Is Positive)** ## **Chorionic Villus Sampling (CVS)** * **10–13+6 weeks** * Transcervical or transabdominal * Results: karyotype, microarray * Miscarriage risk: **~0.2–0.3%** ## **Amniocentesis** * **≥15 weeks** * Lower miscarriage risk: **0.1–0.2%** ## **Rapid tests** * **FISH** (24–48 hrs): detects T21, T18, T13 * **Microarray**: detects microdeletions/duplications --- # **10. Combined Detection Performance** | Test | Detection rate for T21 | | ------------------------ | ---------------------- | | First trimester combined | 85–90% | | Quadruple test | 75% | | Integrated screening | 94–95% | | **NIPT** | **>99%** | NIPT is **preferred**, especially for high-risk pregnancies. --- # **11. When to Offer NIPT (Indications)** * Maternal age ≥35 yrs * Previous trisomy pregnancy * Abnormal ultrasound markers * Positive biochemical screen * IVF pregnancies (optional but recommended) * Parental chromosomal rearrangement (screening may be inadequate → offer diagnostic test) --- # **12. Management Algorithm (Simplified)** ### **STEP 1: First antenatal visit** * Counsel regarding available screening methods * Offer **NIPT** to all (optimal) ### **STEP 2: If NT scan & biochemistry done** * **High-risk → NIPT or CVS** * **Intermediate risk → NIPT** * **Low risk → routine care** ### **STEP 3: Anomaly scan** * If any major structural abnormality → **Diagnostic test (CVS/Amniocentesis)** irrespective of NIPT result ### **STEP 4: If NIPT positive** * **Never terminate pregnancy based on NIPT alone** * Perform **confirmatory CVS/Amniocentesis** --- # **13. Counseling Points** * Screening ≠ diagnosis * Explain detection rates and false positives * Invasive diagnostic tests carry small miscarriage risks * A normal screen reduces but **does not eliminate** risk * Final decision is patient-centered --- # **14. Key Exam High-Yield Points** * **Most sensitive screening test:** NIPT * **Earliest diagnostic test:** CVS * **Best time for NT scan:** 11–13+6 weeks * **AFP ↑:** NTD, abdominal wall defects, incorrect dating * **AFP ↓ + hCG ↑ + uE3 ↓:** Trisomy 21 * **Choroid plexus cyst:** Trisomy 18 marker * **Absent nasal bone:** Down syndrome strongest soft marker * **Echogenic bowel:** Trisomy 21, CMV, CF ---
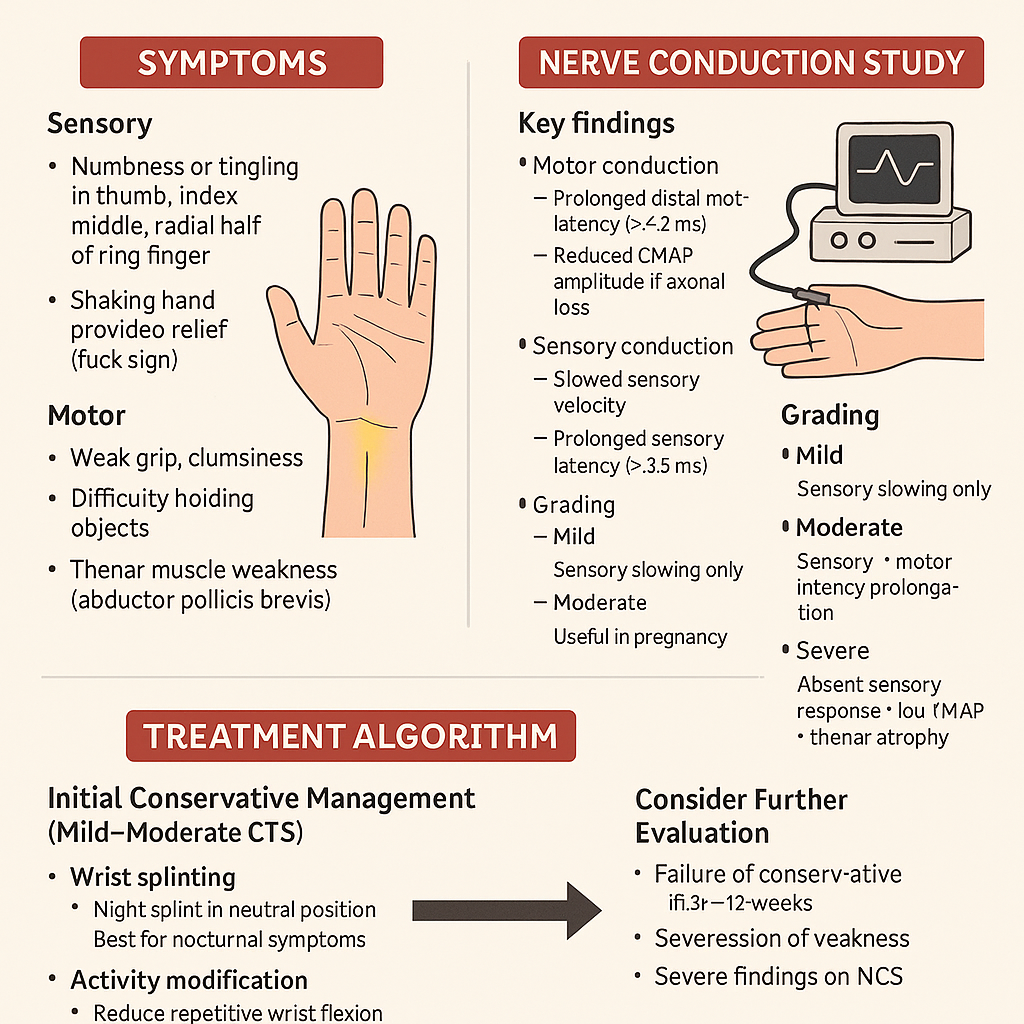
Carpal Tunnel Syndrome: Symptoms, Nerve Conduction Study & Treatment Algorithm
# **Carpal Tunnel Syndrome (CTS): Symptoms, Nerve Conduction Study & Treatment Algorithm** ## **Definition** Carpal Tunnel Syndrome is **median nerve compression** at the level of the wrist within the **carpal tunnel**, leading to sensory and motor dysfunction in the **median nerve distribution**. --- # **Pathophysiology** * The **carpal tunnel** is a rigid space bordered by carpal bones and the **transverse carpal ligament**. * Conditions causing tunnel **volume increase** or **nerve vulnerability** → median nerve ischemia + demyelination. * Chronic compression → **axonal loss** → persistent weakness and atrophy. --- # **Causes / Risk Factors** ### **Local / Mechanical** * Repetitive wrist flexion/extension * Vibrating tool use * Wrist fractures/dislocations * Ganglion cysts, synovitis ### **Systemic** * Diabetes mellitus * Hypothyroidism * Pregnancy (fluid retention) * Rheumatoid arthritis * Obesity * Amyloidosis --- # **Clinical Features** ### **Symptoms** **Sensory:** * Numbness/tingling in **thumb, index, middle, radial half of ring finger** * Symptoms worse at **night** * **Shaking hand provides relief** (flick sign) **Motor:** * Weak grip, clumsiness * Difficulty holding objects * **Thenar muscle weakness** (abductor pollicis brevis) **Autonomic signs (less common):** * Dryness of skin over lateral 3½ fingers --- ### **Physical Examination** * **Tinel’s sign:** Tapping over carpal tunnel → tingling in median nerve area * **Phalen’s test:** Forced wrist flexion for 60 sec → reproduces symptoms * **Durkan’s test (carpal compression test):** Direct pressure over the tunnel → most sensitive * Thenar muscle **atrophy** in advanced disease --- # **Nerve Conduction Study (NCS) — Key Findings** NCS is the **gold standard**. ### **Motor conduction** * Prolonged **distal motor latency** (> 4.2 ms) of median nerve * Reduced CMAP amplitude if axonal loss ### **Sensory conduction** * Slowed sensory velocity * Prolonged **sensory latency** (> 3.5 ms) * Reduced SNAP amplitude ### **Comparison tests** * Median vs ulnar sensory latency to ring finger * Median–radial latency difference to thumb * Very sensitive in early disease ### **Grading** * **Mild:** Sensory slowing only * **Moderate:** Sensory + motor latency prolongation * **Severe:** Absent sensory response + low CMAP + thenar atrophy --- # **Diagnosis** * Clinical examination + NCS * Ultrasound: Median nerve cross-sectional area > **9–10 mm²** at carpal tunnel inlet * X-ray only if trauma suspected * Rule out differentials: cervical radiculopathy (C6), pronator syndrome, diabetic polyneuropathy --- # **Treatment Algorithm (Stepwise)** ## **1. Initial Conservative Management (Mild–Moderate CTS)** ### **a. Wrist Splinting** * **Night splint** in neutral position * Best first-line for nocturnal symptoms ### **b. Activity Modification** * Reduce repetitive wrist flexion * Ergonomic adjustments ### **c. NSAIDs** * Provides symptom relief, but **does not alter nerve pathology** ### **d. Corticosteroid Injection** * Local steroid injection gives **weeks–months of relief** * Useful in pregnancy * Avoid frequent injections (>3/year) --- ## **2. Consider Further Evaluation** * Failure of conservative therapy in **6–12 weeks** * Progression of weakness * Severe findings on NCS --- ## **3. Definitive Treatment — Surgery** ### **Surgical Indication** * Persistent symptoms despite conservative therapy * Severe CTS (thenar atrophy or axonal loss on NCS) * Recurrent symptoms significantly affecting function ### **Procedure** **Carpal Tunnel Release (CTR)** * Cut the transverse carpal ligament to decompress the median nerve * Approaches: **open** or **endoscopic** ### **Outcomes** * Excellent symptom improvement in majority * Thenar strength recovery depends on duration of compression * Recurrence is uncommon --- # **Prognosis** * Early-stage CTS responds well to conservative therapy * Long-standing compression with axonal damage → incomplete recovery * Diabetes: slower improvement * Pregnancy: symptoms often resolve postpartum --- # **Red Flags (Suggest Alternative Diagnosis)** * Whole-hand numbness (not median distribution) * Neck pain + hand paresthesia → cervical radiculopathy * Symptoms not affected by wrist position * Marked weakness without sensory loss → motor neuron or peripheral nerve disorder ---
Osteoporosis: Risk Factors, DEXA Scan Interpretation & Best Drug Therapy 2025
--- # **Osteoporosis: Risk Factors, DEXA Scan Interpretation & Best Drug Therapy 2025** ## **Definition** Osteoporosis is a systemic skeletal disorder characterized by **low bone mass**, **microarchitectural deterioration**, and **increased fracture risk**, commonly affecting postmenopausal women and elderly men. --- # **Pathophysiology** * **Increased bone resorption** vs **decreased bone formation**. * Loss of **trabecular connectivity**, thinning of cortical bone. * Estrogen deficiency → ↑ osteoclast activity. * Age-related decline in osteoblast function. * Secondary causes involve hormonal, nutritional, renal, GI, or drug-induced factors. --- # **Risk Factors** ### **Non-modifiable** * Age > 65 (women), > 70 (men) * Female sex * Postmenopausal status * Family history of hip fracture * Low BMI (<19) ### **Modifiable** * Smoking, alcohol intake >3 units/day * Sedentary lifestyle * Low calcium/vitamin D intake * Poor sunlight exposure ### **Secondary Causes** * Endocrine: Hyperthyroidism, hyperparathyroidism, Cushing, hypogonadism * GI: Malabsorption, celiac disease, bariatric surgery * Renal: CKD–mineral bone disorder * Drugs: **Steroids**, PPIs, anticonvulsants, heparin, aromatase inhibitors * Rheumatologic: RA, SLE --- # **Clinical Features** * Usually **asymptomatic** until fracture * Fragility fractures: vertebral (most common), hip, forearm * Height loss, kyphosis, back pain * Decreased mobility and functional impairment --- # **Diagnosis** ## **1. DEXA Scan (Dual-Energy X-Ray Absorptiometry)** ### **T-Score Interpretation** | T-Score | Interpretation | | ---------------------------------- | ----------------------- | | **≥ –1.0** | Normal | | **–1.0 to –2.5** | **Osteopenia** | | **≤ –2.5** | **Osteoporosis** | | **≤ –2.5 with fragility fracture** | **Severe Osteoporosis** | ### **Sites to Measure** * **Lumbar spine (L1–L4)** * **Total hip** * **Femoral neck** ### **When to Repeat** * Every **1–2 years** depending on therapy response. --- ## **2. FRAX Score** Estimates 10-year risk of **major osteoporotic fracture** and **hip fracture** using age, sex, BMI, and clinical risk factors. **Treatment thresholds (India/Asia 2025 recommendations):** * Major fracture risk ≥20% * Hip fracture risk ≥3% --- # **Investigations for Secondary Causes** * Calcium, phosphate * Vitamin D (25-OH) * PTH * TSH * Renal & liver function * Testosterone (men) * SPEP if myeloma suspected --- # **Management** ## **1. Non-Pharmacologic** * Weight-bearing exercises * Smoking/alcohol cessation * Calcium 1200 mg/day (diet + supplement) * Vitamin D3 800–2000 IU/day * Fall-prevention strategies --- # **2. Pharmacologic Therapy (Updated 2025)** **A. First-Line Agents** ### **⬤ Bisphosphonates (Alendronate, Risedronate, Zoledronic acid)** * **MOA:** Inhibit osteoclast-mediated bone resorption * **Dosing:** * Alendronate 70 mg weekly * Risedronate 35 mg weekly * Zoledronic acid 5 mg IV yearly * **AEs:** Esophagitis, hypocalcemia, atypical femur fractures (long-term), ONJ * **Contraindications:** eGFR <35 mL/min, esophageal motility disorders * **Monitoring:** Calcium, vitamin D, dental evaluation * **Counselling:** Take fasting with water; remain upright 30–60 mins. ### **⬤ Denosumab** * **MOA:** RANKL monoclonal antibody → ↓ osteoclast survival * **Dose:** 60 mg SC every 6 months * **AEs:** Hypocalcemia, infections, ONJ, rebound fractures if stopped * **Important:** Must transition to bisphosphonate when discontinuing. --- **B. Anabolic Agents (Severe or High-Risk Osteoporosis)** ### **⬤ Teriparatide / Abaloparatide** * **MOA:** PTH analog → stimulates osteoblast activity * **Dose:** 20 µg SC daily * **Duration:** Max 24 months * **AEs:** Hypercalcemia, leg cramps * **Use when:** T-score < –3.0, multiple fractures, or failure of antiresorptives. ### **⬤ Romosozumab (2025 availability improving)** * **MOA:** Sclerostin inhibitor → ↑ bone formation + ↓ resorption * **Dose:** 210 mg SC monthly for 12 months * **Contra:** Recent MI/stroke * **AEs:** CV risk, ONJ, atypical femur fractures --- **C. SERMs (Raloxifene)** * **Useful in younger postmenopausal women** * Prevents vertebral fractures only * AEs: Hot flashes, VTE risk --- # **Treatment Algorithm 2025** 1. **Low risk / Osteopenia:** * Lifestyle + calcium/Vit D * Consider bisphosphonate if FRAX above threshold 2. **Moderate to high risk:** * Start bisphosphonate (first-line) * Reassess DEXA at 1–2 years 3. **Very high risk or severe osteoporosis:** * Start **anabolic agent** (teriparatide or romosozumab) * Follow with antiresorptive agent for consolidation 4. **Secondary osteoporosis:** * Treat underlying cause (thyroid, steroids, malabsorption, etc.) --- # **Monitoring** * DEXA every 12–24 months * Serum calcium & vitamin D periodically * Monitor compliance and adverse effects --- # **Long-Tail SEO Tags (comma separated)** osteoporosis risk factors 2025, updated osteoporosis treatment guidelines, dexa scan interpretation chart, osteoporosis drugs comparison 2025, best medicine for osteoporosis 2025, romosozumab indications 2025, teriparatide dosing neet pg, osteoporosis in postmenopausal women, how to read dexa scan results, osteoporosis vs osteopenia differentiation, fragility fracture management, frx score osteoporosis threshold, bisphosphonate contraindications, denosumab side effects rebound fractures, osteoporosis prevention diet exercise ---
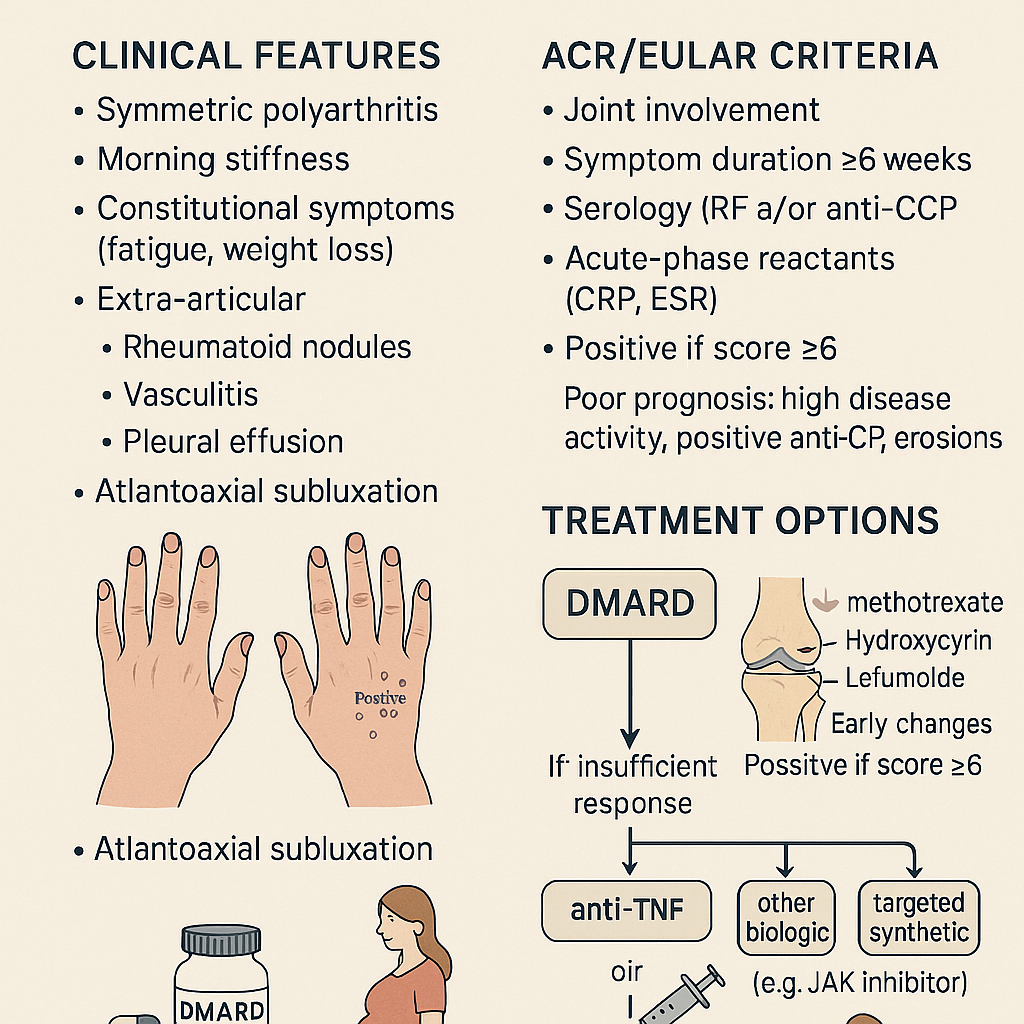
Rheumatoid Arthritis: Clinical Features, ACR/EULAR Criteria & Treatment Options
# **RHEUMATOID ARTHRITIS (RA)** **Clinical Features • ACR/EULAR 2010 Criteria • Diagnosis • Management (stepwise) • Drugs with MoA, dosing, AEs, contraindications, interactions, monitoring & counselling** --- # **1. Definition** Rheumatoid arthritis is a **chronic, systemic, autoimmune inflammatory polyarthritis** primarily affecting **synovial joints**, causing **persistent symmetric polyarthritis**, progressive joint destruction, disability, and extra-articular complications. It is mediated by **autoantibodies (RF, anti-CCP)** and **pro-inflammatory cytokines (TNF-α, IL-6, IL-1)**. --- # **2. Pathophysiology (Short but Complete)** * Genetic: **HLA-DRB1 shared epitope** strongly associated * Autoantibodies: **RF (IgM anti-Fc)** and **anti-CCP** (highly specific) * Inflammatory cascade → **synovial hyperplasia (pannus formation)** → cartilage erosion → bone destruction * Cytokines: **TNF-α, IL-6, IL-1**, JAK-STAT pathway activation * Extra-articular: vasculitis, nodules, ILD, anemia of chronic disease, scleritis * Accelerated **atherosclerosis** → ↑ CV mortality --- # **3. Clinical Features** ## **A. Articular** * **Symmetric small joint polyarthritis** (MCP, PIP, wrists; usually spares DIP) * **Morning stiffness > 1 hour** * Joint tenderness, boggy swelling * **Warm joints but not red** * **Deformities** (late): * Ulnar deviation * Swan-neck deformity * Boutonnière deformity * Z-thumb deformity * Reduced grip strength * In advanced disease: rheumatoid nodules, tendon rupture (e.g., **extensor tendon**) ## **B. Extra-articular** * **Rheumatoid nodules** * **Felty syndrome**: RA + neutropenia + splenomegaly * Ocular: **scleritis, episcleritis, keratoconjunctivitis sicca** * Pulmonary: **ILD, pleural effusion (exudative, low glucose)** * Cardiac: **pericarditis, ↑ CAD risk** * Hematology: anemia of chronic disease, thrombocytosis * Neurological: carpal tunnel syndrome, cervical spine (C1–C2) subluxation * Skin: vasculitic ulcers --- # **4. Investigations & Diagnosis** ### **A. Blood Tests** * **ESR/CRP** ↑ * **RF** positive in ~70–80% * **Anti-CCP**: highly specific (~95%), predicts severe disease * **CBC**: anemia of chronic disease, thrombocytosis * **LFT/RFT** baseline before DMARD therapy ### **B. Imaging** * **X-ray early**: soft tissue swelling, peri-articular osteopenia * **X-ray late**: joint space narrowing, erosions * **Ultrasound / MRI**: detects early synovitis & erosions --- # **5. ACR/EULAR 2010 Classification Criteria for RA** A score **≥ 6/10 = definite RA** ### **A. Joint involvement (0–5 points)** * 1 large joint → 0 * 2–10 large joints → 1 * 1–3 small joints → 2 * 4–10 small joints → 3 * > 10 joints (≥1 small) → 5 ### **B. Serology (0–3 points)** * RF negative & anti-CCP negative → 0 * Low-positive RF or low-positive anti-CCP → 2 * High-positive RF or anti-CCP → 3 ### **C. Acute-phase reactants (0–1 point)** * Normal ESR/CRP → 0 * Abnormal ESR/CRP → 1 ### **D. Duration of symptoms (0–1 point)** * <6 weeks → 0 * ≥6 weeks → 1 --- # **6. Differential Diagnoses** * Osteoarthritis * Psoriatic arthritis * SLE arthritis * Reactive arthritis * Viral polyarthritis (parvovirus B19, chikungunya) * Gout/pseudogout * Polymyalgia rheumatica --- # **7. Management (Stepwise & Evidence-Based)** ## **A. General Principles** * **Early aggressive treatment** with DMARDs * Aim: **remission or low disease activity** * Regular **DAS28** monitoring * Combination DMARDs if inadequate response * Avoid long-term steroids --- # **8. Pharmacologic Treatment (Full drug-level details)** # **1) First-line: Conventional DMARDs** --- ## **A. Methotrexate (MTX) – cornerstone** **Indication:** First-line DMARD for all moderate-severe RA **Mechanism:** Inhibits dihydrofolate reductase → ↓ purine synthesis; ↑ adenosine (anti-inflammatory) **Dose:** * Start 7.5–15 mg once weekly → titrate to **25 mg weekly**; give **folic acid 1 mg/day** **PK:** Hepatic metabolism, renal excretion **Common AEs:** GI upset, stomatitis, hair loss **Serious AEs:** Hepatotoxicity, myelosuppression, pneumonitis **Contraindications:** Pregnancy, liver disease, alcohol use disorder, severe renal impairment **Interactions:** TMP-SMX ↑ MTX toxicity; avoid NSAID excess **Monitoring:** CBC, LFT, RFT every 6–12 weeks **Counselling:** Once weekly dosing, avoid alcohol, report dyspnea --- ## **B. Leflunomide** **MoA:** Inhibits dihydroorotate dehydrogenase → ↓ pyrimidine synthesis **Dose:** 10–20 mg daily **AEs:** Hepatotoxicity, diarrhea, alopecia, teratogenic **Contra:** Pregnancy; need cholestyramine washout **Monitoring:** CBC, LFT every 8 weeks --- ## **C. Sulfasalazine** **MoA:** Anti-inflammatory; modulates cytokines **Dose:** 500 mg/day → 2–3 g/day **AEs:** Rash, GI upset, reversible oligospermia **Contra:** Sulfa allergy **Monitoring:** CBC, LFT --- ## **D. Hydroxychloroquine** **MoA:** Inhibits antigen presentation & TLR pathways **Dose:** 200–400 mg/day **AEs:** Retinopathy (dose-dependent) **Monitoring:** Baseline eye exam + annual screening after 5 yrs **Use:** Mild RA or combination therapy --- # **2) Biologic DMARDs (if inadequate response to MTX)** --- ## **A. Anti-TNF Agents** * **Etanercept** * **Infliximab** * **Adalimumab** * **Golimumab** * **Certolizumab** **MoA:** TNF-α blockade **AEs:** TB reactivation, infections, demyelination, CHF worsening **Contra:** Active infection, demyelinating disease **Monitoring:** TB screening, CBC, LFT **Counselling:** Report fever; maintain vaccination --- ## **B. Anti-IL-6 (Tocilizumab, Sarilumab)** **MoA:** IL-6 receptor blockade **AEs:** ↑ cholesterol, infections, GI perforation (esp. diverticulitis) --- ## **C. Anti-CD20 (Rituximab)** **MoA:** B-cell depletion **Use:** Refractory RA or when biologics contraindicated **AEs:** Infusion reactions, hepatitis B reactivation --- ## **D. CTLA-4 Fusion Protein (Abatacept)** **MoA:** Inhibits T-cell activation **AEs:** Infections, COPD exacerbation --- # **3) Targeted Synthetic DMARDs – JAK Inhibitors** * **Tofacitinib** * **Baricitinib** * **Upadacitinib** **MoA:** JAK-STAT inhibition → ↓ cytokine signaling **AEs:** Herpes zoster, ↑ LDL/HDL, thrombosis risk **Monitoring:** CBC, lipids, LFT **Counselling:** Vaccinate for zoster before therapy --- # **4) Glucocorticoids** * Used as **bridge therapy** until DMARDs act * Dose: **Prednisolone 5–10 mg/day short-term** * AEs: osteoporosis, weight gain, infection, HTN * Avoid chronic use * Provide **calcium + vitamin D** --- # **5) NSAIDs** * Symptomatic relief only * Do NOT prevent joint damage * Contra: renal disease, peptic ulcer, CVD --- # **9. Non-Pharmacologic Management** * Physiotherapy + joint-protection exercises * Smoking cessation (smoking worsens RA) * Weight optimisation * Vaccination: influenza, pneumococcal before biologics * Occupational therapy * Surgery: joint replacement in advanced destruction --- # **10. Follow-Up & Monitoring** * DAS28 scoring every 3 months * Monitor DMARD toxicity: CBC, LFT, RFT * Eye exams for hydroxychloroquine * TB screening annually for biologics --- # **11. Prognostic Factors** **Poor prognosis indicators:** * High RF/anti-CCP titers * Early erosions on X-ray * High disease activity (DAS28) * Extra-articular disease * Smoking * Early disability ---
Browse by Medical Category
Explore content organized by medical specialties and systems