Clinical videos + HTML notes for NEET PG-ready revision.
Streamora lets you upload case-based videos, attach rich HTML notes, like and comment on other clinicians’ posts, follow creators and save structured exam-oriented pearls – all mobile-first and SEO-ready.
Why Streamora stands out for NEET PG aspirants: Unlike generic apps, we focus on high-yield topics like labour stages (from first to fourth, with management pitfalls), Rh-negative pregnancies (anti-D prophylaxis timing), and anatomy pearls (e.g., sacral hiatus for caudal blocks). Our community-driven notes include real residency cases—e.g., "Missed Rh isoimmunization leading to hydrops fetalis"—with attached flowcharts and MCQ-style tags for quick revision. Free, ad-light, and built by med students for med students.
Latest Medical Posts
High-yield medical discussions, NEET PG-flavoured notes and short clinical cases from all users.
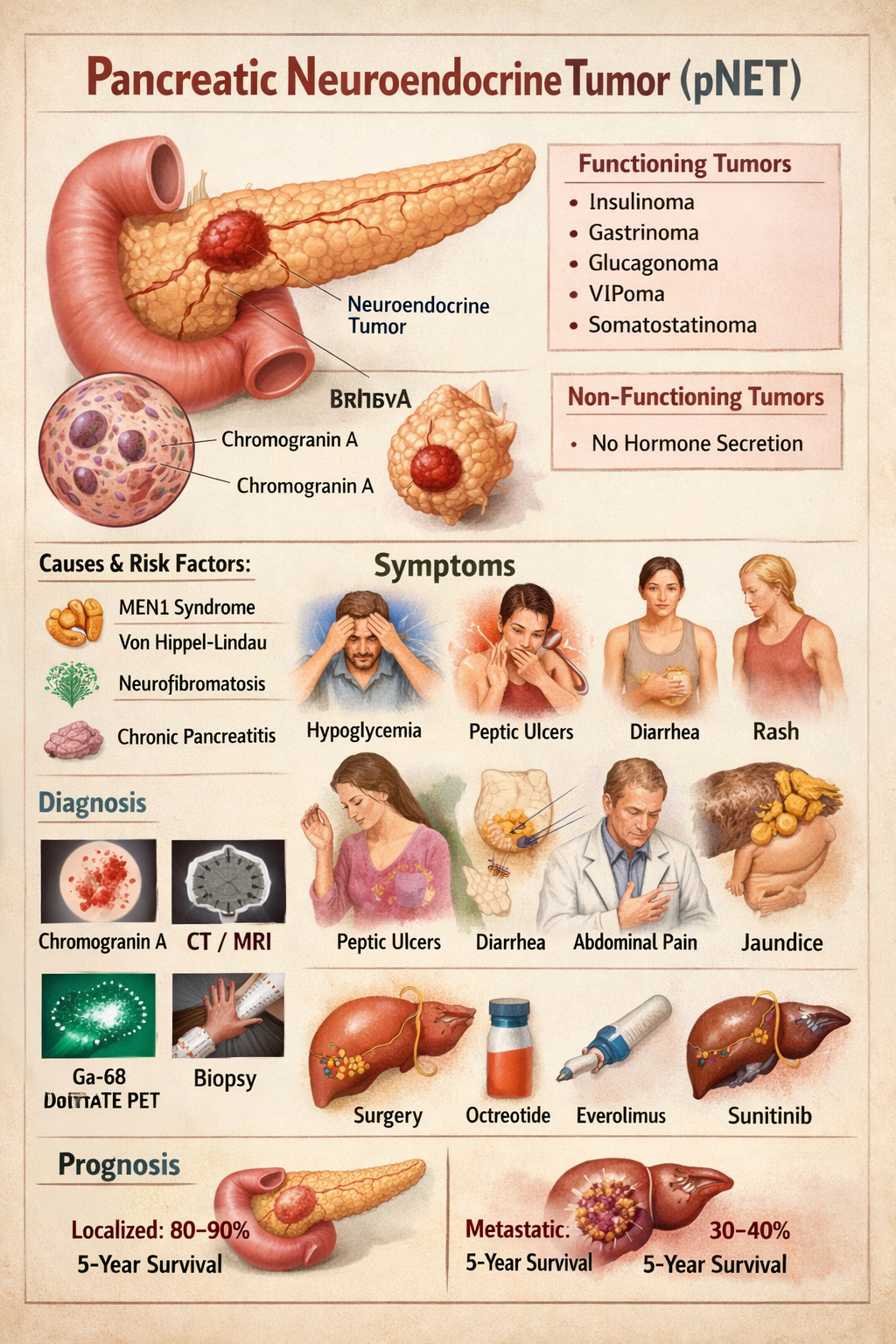
Pancreatic Neuroendocrine Tumor Symptoms Diagnosis Treatment Prognosis
--- # **PANCREATIC NEUROENDOCRINE TUMOR (pNET)** --- ## **1. Definition** Pancreatic neuroendocrine tumors (pNETs) are **neoplasms arising from endocrine (islet) cells of the pancreas** that secrete peptide hormones or amines. They are biologically distinct from pancreatic adenocarcinoma and may be **functioning (hormone-secreting)** or **non-functioning**. --- ## **2. Pathophysiology** pNETs originate from **enterochromaffin cells** of pancreatic islets. They show: * **Neuroendocrine differentiation** * **Dense-core secretory granules** * **Expression of chromogranin A and synaptophysin** Tumor behavior depends on: * **Hormone secretion** * **Tumor size** * **Ki-67 index (mitotic rate)** * **Invasion and metastasis** Tumors may be: * **Well differentiated (NET G1–G3)** * **Poorly differentiated (Neuroendocrine carcinoma)** MEN1 mutation commonly involved → parathyroid, pituitary, pancreas tumors. --- ## **3. Classification** ### **A. By hormone secretion** | Type | Hormone | | --------------- | ------------ | | Insulinoma | Insulin | | Gastrinoma | Gastrin | | Glucagonoma | Glucagon | | VIPoma | VIP | | Somatostatinoma | Somatostatin | | Non-functioning | None | ### **B. By WHO grading** | Grade | Ki-67 | | ----- | ----- | | G1 | <3% | | G2 | 3–20% | | G3 | >20% | --- ## **4. Causes and Risk Factors** * MEN-1 syndrome * Von Hippel–Lindau * Neurofibromatosis-1 * Tuberous sclerosis * Smoking * Chronic pancreatitis --- ## **5. Clinical Features** ### **A. Insulinoma** * Hypoglycemia * Sweating * Palpitations * Confusion * Weight gain ### **B. Gastrinoma (Zollinger-Ellison)** * Severe recurrent peptic ulcers * Diarrhea * GERD ### **C. Glucagonoma** * Diabetes * Necrolytic migratory erythema * Weight loss * Anemia ### **D. VIPoma** * Profuse watery diarrhea * Hypokalemia * Achlorhydria ### **E. Somatostatinoma** * Diabetes * Gallstones * Steatorrhea ### **F. Non-functioning** * Abdominal pain * Weight loss * Jaundice * Abdominal mass * Metastasis symptoms --- ## **6. Investigations** ### **Blood Tests** | Test | Use | | ------------------ | --------------- | | Chromogranin-A | Tumor marker | | Insulin, C-peptide | Insulinoma | | Gastrin | Gastrinoma | | Glucagon | Glucagonoma | | VIP | VIPoma | | Somatostatin | Somatostatinoma | | Fasting glucose | Hypoglycemia | ### **Imaging** * Contrast CT * MRI pancreas * Endoscopic ultrasound (best for small tumors) * Ga-68 DOTATATE PET-CT (gold standard) * Octreoscan ### **Biopsy** * EUS-guided biopsy * Ki-67 index --- ## **7. Differential Diagnosis** * Pancreatic adenocarcinoma * Islet cell hyperplasia * Metastatic carcinoid * Chronic pancreatitis * Insulin autoimmune syndrome --- ## **8. Management** ### **A. Curative – Surgery** * Enucleation (small insulinomas) * Distal pancreatectomy * Whipple procedure * Liver metastasis resection ### **B. Medical Therapy** Used when metastatic, unresectable or hormone excess. --- ## **9. Drugs Used** ### **1. Octreotide** **Indication:** Hormone control and tumor stabilization **Mechanism:** Somatostatin analog → inhibits hormone secretion **Dose:** Adult: 100–500 mcg SC 2–3 times/day or 20–30 mg IM monthly Paediatric: 1–10 mcg/kg/day **Adverse effects:** Gallstones, diarrhea, hyperglycemia **Contraindication:** Severe gallbladder disease **Monitoring:** LFT, glucose **Counsel:** May cause GI upset --- ### **2. Lanreotide** Same as octreotide Dose: 120 mg SC every 4 weeks --- ### **3. Everolimus** **Indication:** Advanced pNET **Mechanism:** mTOR inhibitor **Dose:** 10 mg daily **Adverse:** Mouth ulcers, hyperglycemia, infections **Contra:** Active infection **Monitor:** CBC, glucose **Counsel:** Avoid live vaccines --- ### **4. Sunitinib** **Indication:** Metastatic pNET **Mechanism:** VEGF receptor inhibitor **Dose:** 37.5 mg daily **Adverse:** Hypertension, fatigue **Contra:** Cardiac failure **Monitor:** BP, ECG --- ### **5. Diazoxide (for insulinoma)** **Mechanism:** Inhibits insulin release **Dose:** 100–600 mg/day **Adverse:** Fluid retention, hyperglycemia **Monitor:** Glucose, edema --- ### **6. Streptozocin + 5-FU (Chemotherapy)** **Indication:** High-grade metastatic disease **Adverse:** Nephrotoxicity, nausea --- ## **10. Non-Pharmacologic** * Surgical resection * Radiofrequency ablation of liver mets * Peptide receptor radionuclide therapy (PRRT) * Dietary glucose support in insulinoma --- ## **11. Prognosis** * Localized pNET: 80–90% 5-year survival * Metastatic: 30–40% Better than pancreatic adenocarcinoma --- ## **12. Key Exam Points** * Insulinoma = most common pNET * Gastrinoma = most malignant * MEN1 = 3 P’s: Parathyroid, Pituitary, Pancreas * Chromogranin A is universal tumor marker * Ga-68 DOTATATE PET = best imaging ---
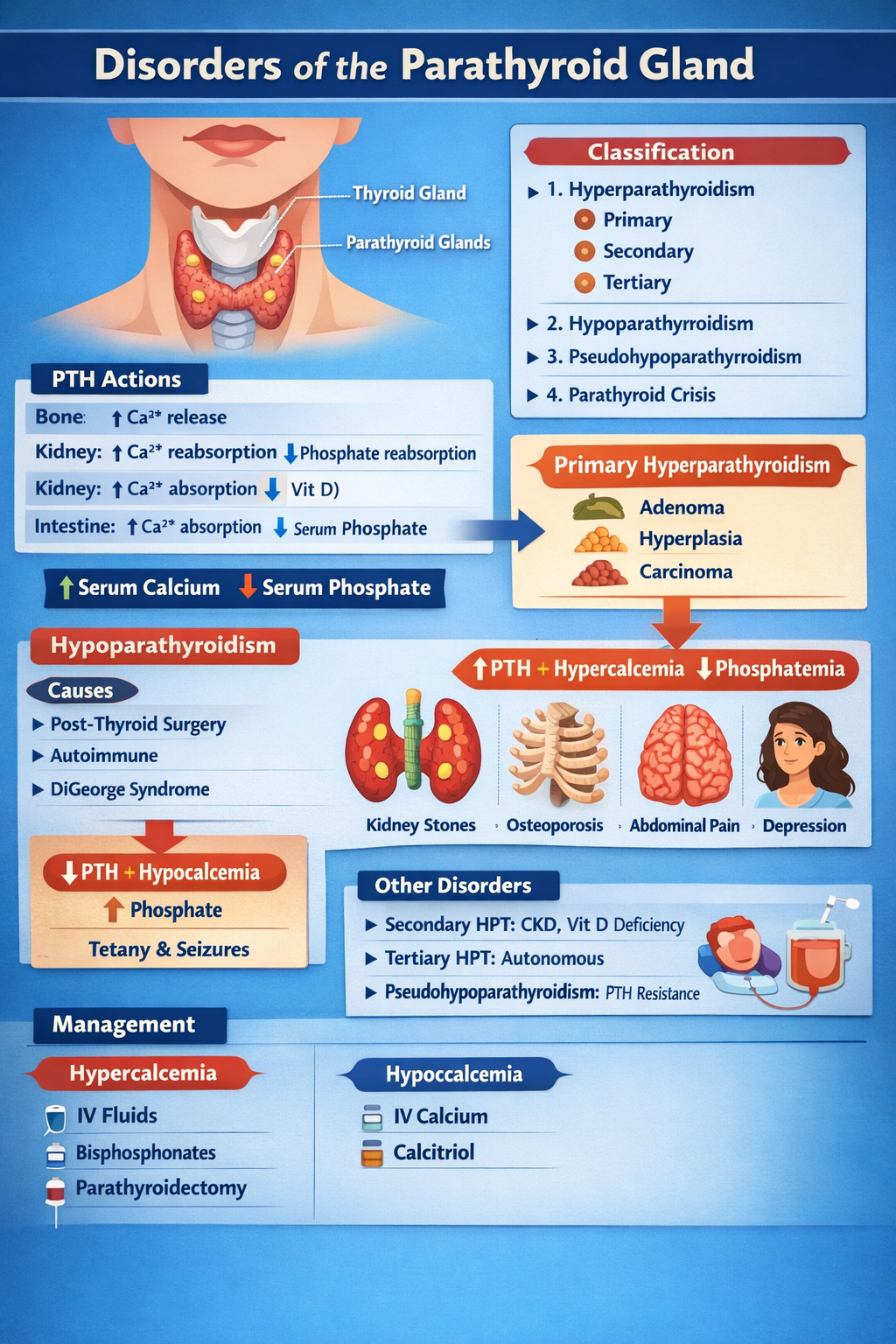
Disorders of Parathyroid Gland Complete Clinical Guide for Medical Students
--- # **DISORDERS OF THE PARATHYROID GLAND** --- ## **1. Physiology of Parathyroid Hormone (PTH)** **Parathyroid glands (4)** → secrete **PTH** → maintain **serum calcium and phosphate balance** ### **Normal actions of PTH** | Target organ | Action | | ------------- | ----------------------------------------------- | | **Bone** | ↑ Osteoclastic bone resorption → ↑ Ca²⁺ release | | **Kidney** | ↑ Ca²⁺ reabsorption, ↓ phosphate reabsorption | | **Kidney** | ↑ 1-α hydroxylase → ↑ calcitriol | | **Intestine** | Indirectly ↑ Ca²⁺ absorption via vitamin D | **Net effect:** **↑ Serum calcium, ↓ serum phosphate** --- # **CLASSIFICATION** 1. **Hyperparathyroidism** * Primary * Secondary * Tertiary 2. **Hypoparathyroidism** 3. **Pseudohypoparathyroidism** 4. **Parathyroid crisis** --- # **PRIMARY HYPERPARATHYROIDISM (PHPT)** ## **Definition** Autonomous excessive PTH secretion → **hypercalcemia** ## **Causes** | Cause | % | | ----------------------- | ------ | | Parathyroid adenoma | 85% | | Parathyroid hyperplasia | 10–15% | | Parathyroid carcinoma | <1% | | MEN-1, MEN-2A | Rare | --- ## **Pathophysiology** Excess PTH → * ↑ Bone resorption → osteoporosis * ↑ Renal Ca reabsorption * ↑ Vitamin D → ↑ gut Ca absorption → **Hypercalcemia + hypophosphatemia** --- ## **Clinical Features** **“Stones, Bones, Groans, Thrones, Psychiatric Overtones”** | System | Features | | ------ | ---------------------------------------------- | | Kidney | Nephrolithiasis, polyuria | | Bone | Bone pain, fractures, osteitis fibrosa cystica | | GIT | Constipation, pancreatitis, peptic ulcer | | CNS | Depression, confusion | | Heart | Short QT | --- ## **Investigations** | Test | Result | | -------------------- | ---------------- | | Serum Ca | ↑ | | Serum phosphate | ↓ | | PTH | ↑ | | ALP | ↑ | | 24-hr urine Ca | ↑ | | DEXA | Osteoporosis | | Neck USG / Sestamibi | Localize adenoma | --- ## **Differential Diagnosis** | Condition | PTH | Ca | | ------------------------ | --- | -------- | | PHPT | ↑ | ↑ | | Malignancy hypercalcemia | ↓ | ↑ | | FHH | ↑ | Normal/↑ | --- ## **Management** ### **A. Acute hypercalcemia** | Step | Treatment | | ---- | ----------------- | | 1 | IV normal saline | | 2 | Loop diuretic | | 3 | IV bisphosphonate | | 4 | Calcitonin | ### **B. Definitive** **Parathyroidectomy** **Indications** * Ca >1 mg/dL above normal * Kidney stones * Osteoporosis * Age <50 --- # **SECONDARY HYPERPARATHYROIDISM** ## **Definition** Compensatory ↑ PTH due to **hypocalcemia** ## **Causes** * Chronic kidney disease (most common) * Vitamin D deficiency * Malabsorption --- ## **Biochemistry** | Parameter | Result | | --------- | ---------- | | Calcium | ↓ | | Phosphate | ↑ (in CKD) | | PTH | ↑ | | Vitamin D | ↓ | --- ## **Management** * Oral calcium * Vitamin D (calcitriol) * Phosphate binders * Dialysis if CKD --- # **TERTIARY HYPERPARATHYROIDISM** Long-standing secondary → autonomous glands | Ca | PTH | | -- | --- | | ↑ | ↑ | **Treatment:** Parathyroidectomy --- # **HYPOPARATHYROIDISM** ## **Definition** Deficient PTH → hypocalcemia ## **Causes** * Post-thyroid surgery (most common) * Autoimmune * DiGeorge syndrome * Hypomagnesemia --- ## **Pathophysiology** Low PTH → ↓ calcium, ↑ phosphate → neuromuscular excitability --- ## **Clinical Features** | Feature | Mechanism | | --------------- | ------------------------------ | | Tetany | Hypocalcemia | | Chvostek sign | Facial nerve hyperexcitability | | Trousseau sign | Carpopedal spasm | | Seizures | Low Ca | | QT prolongation | Hypocalcemia | --- ## **Investigations** | Test | Result | | --------- | -------- | | Ca | ↓ | | Phosphate | ↑ | | PTH | ↓ | | Mg | May be ↓ | --- ## **Management** ### **Acute** IV **calcium gluconate** ### **Chronic** * Oral calcium * Calcitriol --- # **CALCIUM GLUCONATE** | Parameter | Value | | ------------ | -------------------- | | Indication | Acute tetany | | Mechanism | Raises serum Ca | | Dose | 10 ml of 10% IV slow | | Side effects | Arrhythmia | | Monitoring | ECG | --- # **CALCITRIOL (Vitamin D)** | Feature | Detail | | ------------ | -------------------------- | | Action | ↑ Intestinal Ca absorption | | Dose | 0.25–1 mcg/day | | Side effects | Hypercalcemia | | Monitoring | Serum Ca | --- # **PSEUDOHYPOPARATHYROIDISM** ## **Definition** Target organ resistance to PTH | Ca | PTH | Phosphate | | -- | --- | --------- | | ↓ | ↑ | ↑ | ## **Clinical** * Short stature * Round face * Brachydactyly * Mental retardation **Treatment:** Calcium + Vitamin D --- # **PARATHYROID CRISIS** Severe hypercalcemia (>14 mg/dL) ### **Features** * Dehydration * Arrhythmia * Coma ### **Management** 1. IV saline 2. Loop diuretic 3. Calcitonin 4. Bisphosphonates 5. Dialysis if refractory --- # **EXAM PEARLS** | Scenario | Diagnosis | | --------------------------------- | --------------------------- | | High Ca + high PTH | Primary hyperparathyroidism | | Low Ca + high PTH | Secondary HPT | | Low Ca + low PTH | Hypoparathyroidism | | Low Ca + high PTH + short fingers | Pseudohypoparathyroidism | ---
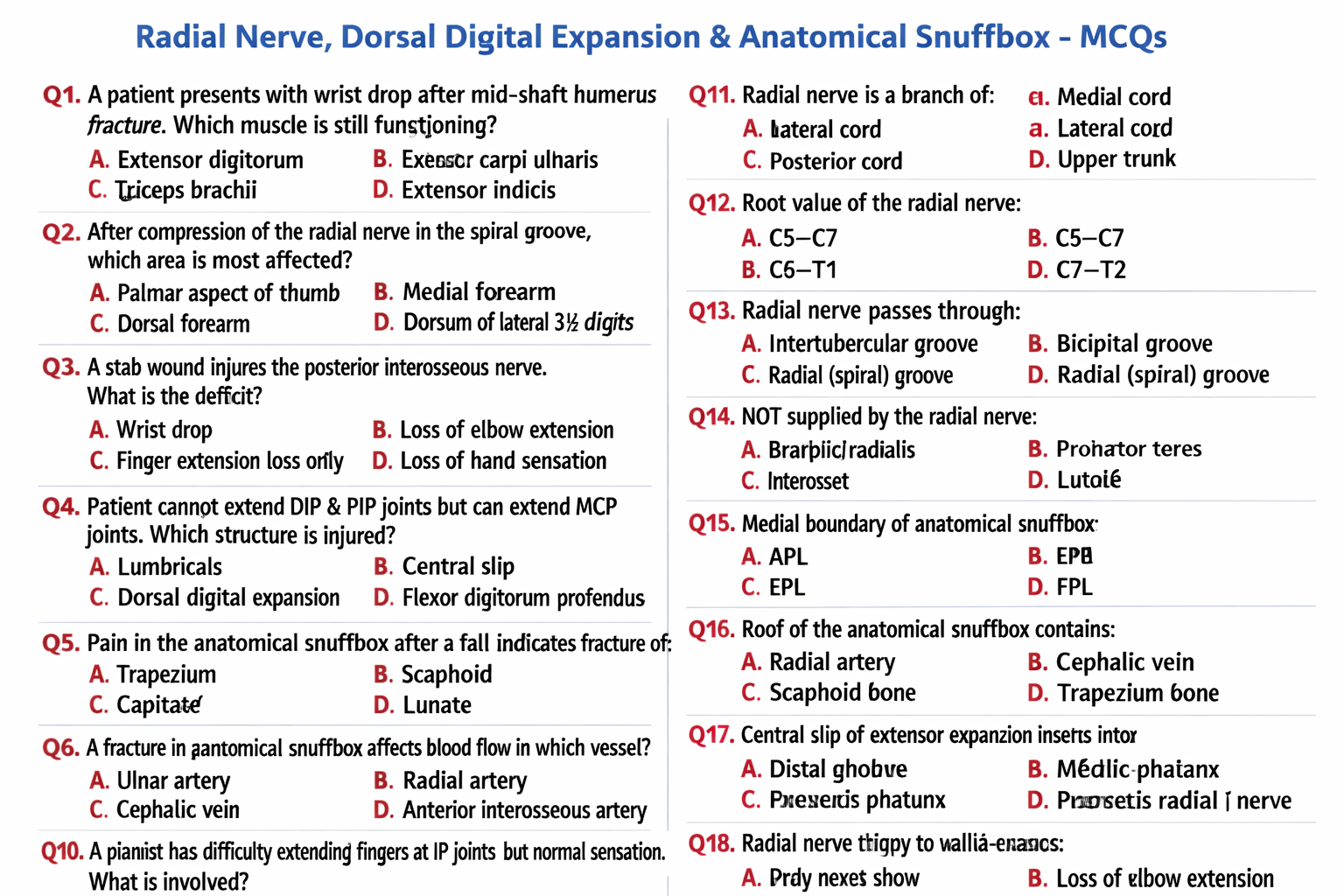
Radial Nerve, Dorsal Digital Expansion and Anatomical Snuffbox Anatomy Explained
Below is a **clear, exam-oriented, complete anatomy note** on **Radial Nerve**, **Dorsal Digital Expansion**, and **Anatomical Snuffbox**. (As requested: **no images**.) --- # **Radial Nerve, Dorsal Digital Expansion, and Anatomical Snuffbox – Complete Anatomy Guide** --- ## **1. Radial Nerve** ### **Definition** The **radial nerve** is the **largest branch of the posterior cord of the brachial plexus**, providing **motor supply to extensor muscles** of the upper limb and **sensory supply to the posterior arm, forearm, and dorsum of the hand**. ### **Root Value** * **C5–T1** --- ### **Origin** * Arises from the **posterior cord of the brachial plexus** --- ### **Course** #### **Axilla** * Lies **posterior to the axillary artery** * Exits the axilla through the **lower triangular space** * Accompanied by the **profunda brachii artery** #### **Arm** * Enters the **radial (spiral) groove** of the humerus * Runs between **medial and lateral heads of triceps** * Supplies **triceps brachii** * Pierces the **lateral intermuscular septum** * Enters the anterior compartment near the lateral epicondyle #### **Cubital Fossa** * Lies **anterior to the lateral epicondyle** * Divides into: * **Superficial branch (sensory)** * **Deep branch (motor → posterior interosseous nerve)** #### **Forearm** * **Deep branch**: * Pierces **supinator** * Continues as **posterior interosseous nerve** * Supplies extensor muscles * **Superficial branch**: * Runs under brachioradialis * Becomes superficial near wrist * Supplies dorsum of hand --- ### **Branches** #### **Motor** * Triceps brachii * Anconeus * Brachioradialis * Extensor carpi radialis longus * All **extensors of wrist and fingers** (via posterior interosseous nerve) #### **Sensory** * Posterior cutaneous nerve of arm * Posterior cutaneous nerve of forearm * Dorsal digital nerves to: * Lateral 3½ digits (proximal parts) --- ### **Applied Anatomy** * **Radial nerve palsy**: * Wrist drop * Loss of finger extension * **Mid-shaft humerus fracture** → injury in radial groove * **Saturday night palsy** → compression in spiral groove --- ## **2. Dorsal Digital Expansion (Extensor Expansion / Hood)** ### **Definition** The **dorsal digital expansion** is a **triangular aponeurotic expansion** on the **dorsum of fingers**, formed mainly by **extensor digitorum tendon**, allowing **coordinated finger movements**. --- ### **Formation** Formed by: * Extensor digitorum tendon * Contributions from: * Lumbricals * Interossei --- ### **Structure** * **Central slip**: * Inserts into base of **middle phalanx** * **Two lateral bands**: * Reunite to insert into **distal phalanx** * Covers the **dorsum of MCP, PIP, and DIP joints** --- ### **Functions** * Extension at: * Metacarpophalangeal (MCP) joints * Interphalangeal (IP) joints * Allows **interossei and lumbricals** to: * Flex MCP * Extend IP joints --- ### **Clinical Importance** * **Mallet finger**: rupture of terminal tendon * **Boutonnière deformity**: rupture of central slip * **Claw hand deformity**: imbalance of intrinsic muscles --- ## **3. Anatomical Snuffbox** ### **Definition** The **anatomical snuffbox** is a **triangular depression** seen on the **lateral aspect of the dorsum of the hand** when the thumb is extended. --- ### **Boundaries** #### **Lateral (Anterior) Boundary** * Abductor pollicis longus * Extensor pollicis brevis #### **Medial (Posterior) Boundary** * Extensor pollicis longus #### **Proximal Boundary** * Styloid process of radius --- ### **Floor** * Scaphoid * Trapezium --- ### **Roof** * Skin * Superficial fascia * Superficial branch of radial nerve * Cephalic vein --- ### **Contents** * **Radial artery** (main content) --- ### **Clinical Importance** * **Scaphoid fracture**: * Tenderness in snuffbox * Risk of avascular necrosis * Radial artery palpation site * IV cannulation landmark --- ## **Quick Exam Correlation Table** | Structure | Key Clinical Point | | ------------------------ | ----------------------------- | | Radial nerve | Wrist drop | | Dorsal digital expansion | Finger extension coordination | | Anatomical snuffbox | Scaphoid fracture tenderness | --- ### **If you want next** * High-yield **MCQs** * **Clinical case scenarios** * **Comparison tables** * **OSCE-ready short notes** Just tell me 👍
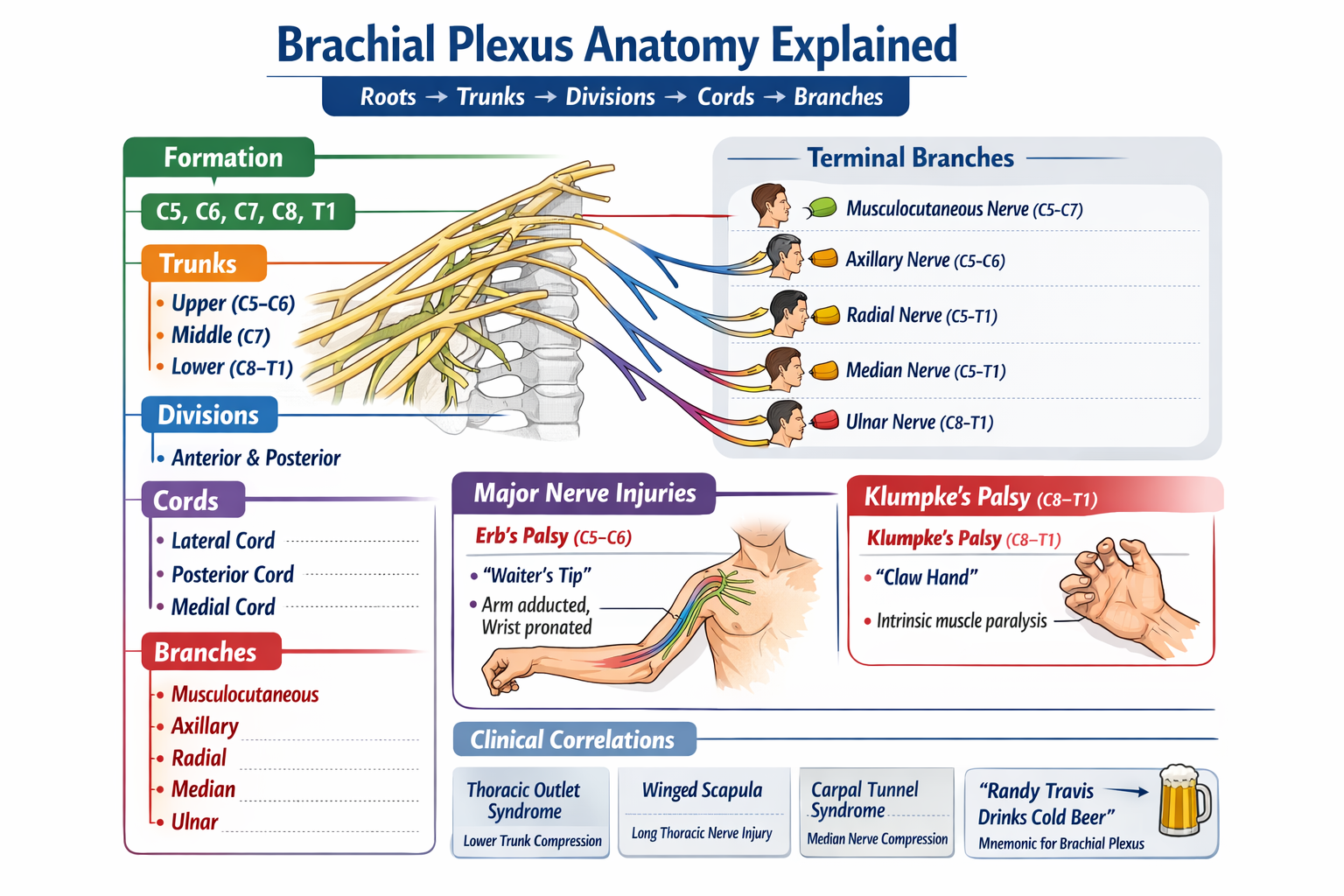
Brachial Plexus Anatomy Explained with Roots Trunks Cords Branches and Clinical Correlations
## **Brachial Plexus – Complete Detailed Anatomy** ### **Definition** The **brachial plexus** is a network of **ventral rami of spinal nerves C5–T1** that provides **motor, sensory, and sympathetic innervation** to the upper limb. --- ## **Formation (Roots → Trunks → Divisions → Cords → Branches)** ### **1. Roots** * **C5, C6, C7, C8, T1** (ventral rami) * Pass between **anterior and middle scalene muscles** in the neck * **Branches from roots:** * **Dorsal scapular nerve (C5)** → Rhomboids, levator scapulae * **Long thoracic nerve (C5–C7)** → Serratus anterior (winged scapula if injured) --- ### **2. Trunks** Formed in the **posterior triangle of the neck** * **Upper trunk:** C5–C6 * **Middle trunk:** C7 * **Lower trunk:** C8–T1 **Branches from trunks:** * **Suprascapular nerve (C5–C6)** → Supraspinatus, infraspinatus * **Nerve to subclavius (C5–C6)** --- ### **3. Divisions** Located **behind the clavicle** * Each trunk divides into: * **Anterior division** → Flexor compartments * **Posterior division** → Extensor compartments * **No branches** arise here --- ### **4. Cords** Named according to relation to the **axillary artery** (in axilla) | Cord | Formation | | ------------------ | ------------------------------------------- | | **Lateral cord** | Anterior divisions of upper + middle trunks | | **Medial cord** | Anterior division of lower trunk | | **Posterior cord** | All posterior divisions | --- ### **5. Terminal Branches** #### **From Lateral Cord** * **Musculocutaneous nerve (C5–C7)** * **Lateral root of median nerve** #### **From Medial Cord** * **Ulnar nerve (C8–T1)** * **Medial root of median nerve** * **Medial cutaneous nerve of arm** * **Medial cutaneous nerve of forearm** #### **From Posterior Cord** * **Axillary nerve (C5–C6)** * **Radial nerve (C5–T1)** --- ## **Major Peripheral Nerves – Functions & Lesions** ### **Musculocutaneous Nerve (C5–C7)** * **Motor:** Biceps, brachialis, coracobrachialis * **Sensory:** Lateral forearm * **Injury:** Weak elbow flexion & supination --- ### **Axillary Nerve (C5–C6)** * **Motor:** Deltoid, teres minor * **Sensory:** Regimental badge area * **Injury:** Surgical neck fracture → loss of shoulder abduction (15–90°) --- ### **Radial Nerve (C5–T1)** * **Motor:** All extensors of arm & forearm * **Sensory:** Posterior arm, forearm, dorsal hand * **Injury:** Wrist drop --- ### **Median Nerve (C5–T1)** * **Motor:** Forearm flexors, thenar muscles * **Sensory:** Lateral 3½ digits (palmar) * **Injury:** Ape hand, loss of pronation, carpal tunnel syndrome --- ### **Ulnar Nerve (C8–T1)** * **Motor:** Intrinsic hand muscles * **Sensory:** Medial 1½ fingers * **Injury:** Claw hand, Froment sign --- ## **Clinical Correlations** ### **Upper Trunk Lesion (Erb Palsy – C5–C6)** * Causes: Birth injury, fall on shoulder * Deformity: **“Waiter’s tip”** * Affected nerves: Axillary, musculocutaneous, suprascapular --- ### **Lower Trunk Lesion (Klumpke Palsy – C8–T1)** * Causes: Traction of abducted arm * Features: * Intrinsic hand muscle paralysis * **Claw hand** * **Horner syndrome** (if T1 sympathetic affected) --- ## **Applied Anatomy** * **Scalene block anesthesia** targets roots/trunks * **Axillary block** targets terminal branches * **Thoracic outlet syndrome** affects lower trunk * **Winged scapula** → Long thoracic nerve injury --- ## **Key Exam Mnemonic** **Roots → Trunks → Divisions → Cords → Branches** **“Randy Travis Drinks Cold Beer”** --- If you want, I can also provide: * **High-yield exam tables** * **Clinical case-based MCQs** * **Dermatome & myotome correlation** * **Pure neuroanatomy vs applied surgery focus** Just tell me 👍
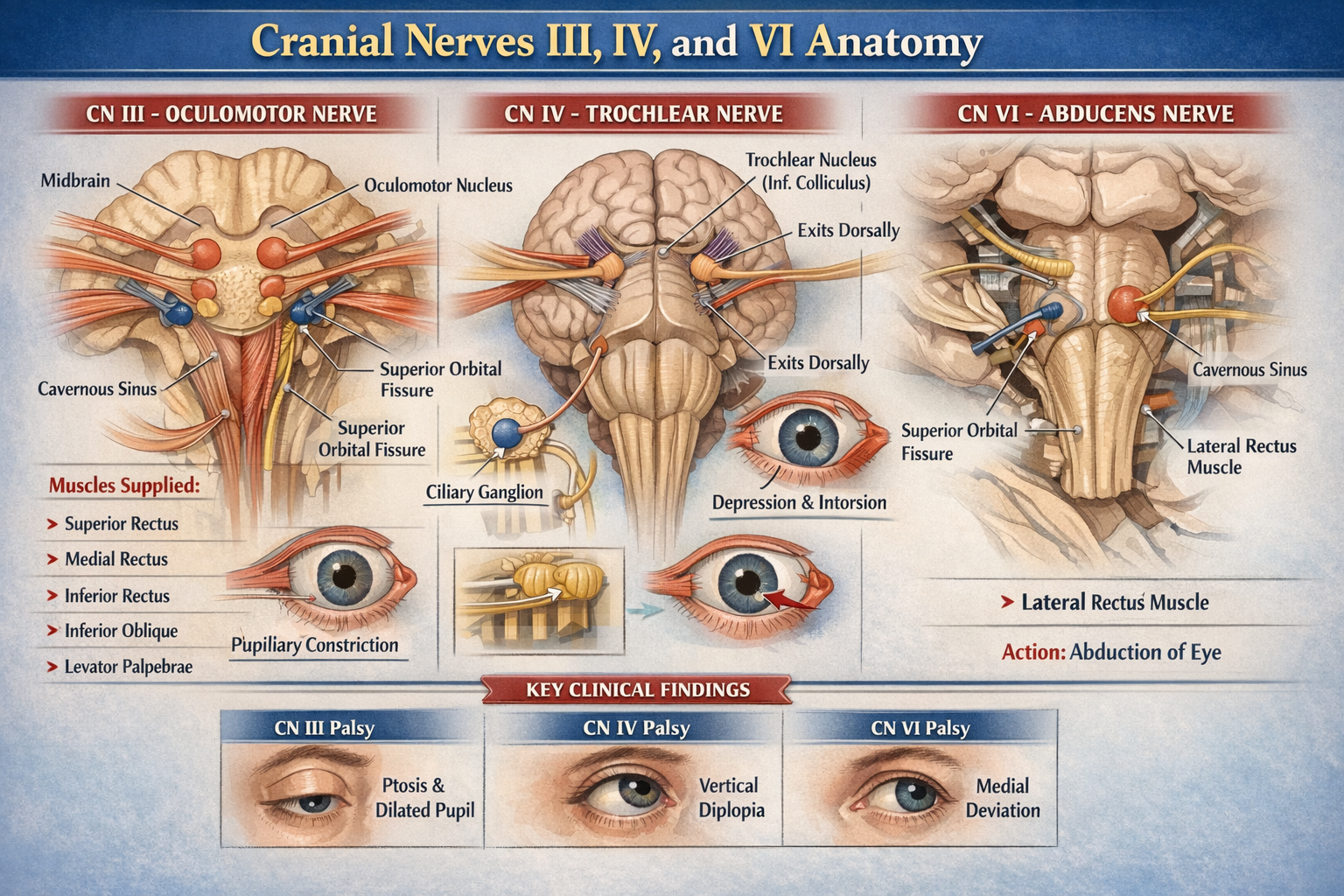
Cranial Nerves III IV VI Anatomy Detailed Overview for Medical Students
Below is a **concise but complete, exam-oriented anatomy reference** for **Cranial Nerves III, IV, and VI** (oculomotor, trochlear, abducens). **No images included**, as requested. --- # Cranial Nerves III, IV, and VI – Detailed Anatomy ## Overview (Common Function) Cranial nerves **III, IV, and VI** are **purely motor nerves** supplying the **extra-ocular muscles** that control eye movements. Cranial nerve III also carries **parasympathetic fibers** for pupil constriction and accommodation. --- ## CRANIAL NERVE III – OCULOMOTOR NERVE ### Functional Components * **Somatic efferent** → extra-ocular muscles * **General visceral efferent (parasympathetic)** → pupil and lens --- ### Nuclei (Midbrain) Located at the **level of the superior colliculus**: 1. **Oculomotor nuclear complex** * Supplies all extra-ocular muscles except SO and LR 2. **Edinger–Westphal nucleus** * Parasympathetic nucleus * Supplies sphincter pupillae and ciliary muscle --- ### Intracranial Course * Emerges from **ventral midbrain** in the **interpeduncular fossa** * Passes between: * **Posterior cerebral artery** * **Superior cerebellar artery** * Runs in **lateral wall of cavernous sinus** * Divides into **superior and inferior divisions** * Enters orbit through **superior orbital fissure** (inside common tendinous ring) --- ### Orbital Course and Branches #### Superior Division * Levator palpebrae superioris * Superior rectus #### Inferior Division * Medial rectus * Inferior rectus * Inferior oblique * Parasympathetic root to **ciliary ganglion** --- ### Parasympathetic Pathway * Edinger–Westphal nucleus → oculomotor nerve * Synapse in **ciliary ganglion** * Postganglionic fibers via **short ciliary nerves** to: * Sphincter pupillae → pupillary constriction * Ciliary muscle → accommodation --- ### Muscles Supplied * Superior rectus * Inferior rectus * Medial rectus * Inferior oblique * Levator palpebrae superioris --- ### Actions * Eye elevation, depression, adduction * Pupillary constriction * Accommodation * Eyelid elevation --- ## CRANIAL NERVE IV – TROCHLEAR NERVE ### Functional Component * **Somatic efferent only** --- ### Nucleus (Midbrain) * Located at **level of inferior colliculus** --- ### Unique Anatomical Features * Only cranial nerve: * That **emerges dorsally** * That **decussates completely** * That has the **longest intracranial course** * That supplies the **contralateral muscle** --- ### Intracranial Course * Exits dorsal midbrain * Winds around brainstem laterally * Passes through: * Cavernous sinus (lateral wall) * Superior orbital fissure (outside common tendinous ring) --- ### Orbital Course * Enters orbit superiorly * Supplies **superior oblique muscle** --- ### Muscle Supplied * **Superior oblique** --- ### Action of Superior Oblique * Intorsion * Depression (especially in adducted eye) * Abduction --- ## CRANIAL NERVE VI – ABDUCENS NERVE ### Functional Component * **Somatic efferent only** --- ### Nucleus (Pons) * Located in **dorsal pons**, beneath **facial colliculus** * Facial nerve fibers loop around abducens nucleus --- ### Intracranial Course * Emerges at **pontomedullary junction** * Ascends along clivus * Sharp bend over **petrous apex** * Passes through **cavernous sinus** (adjacent to internal carotid artery) * Enters orbit via **superior orbital fissure** (inside common tendinous ring) --- ### Orbital Course * Supplies **lateral rectus muscle** --- ### Muscle Supplied * **Lateral rectus** --- ### Action * **Abduction of eyeball** --- ## Summary Table | Cranial Nerve | Nucleus Level | Exit from Brainstem | Muscle Supplied | Main Action | | ------------- | -------------------------- | ----------------------- | -------------------------- | -------------------------------- | | CN III | Midbrain (sup. colliculus) | Ventral | Most EOM + parasympathetic | Eye movement, pupil constriction | | CN IV | Midbrain (inf. colliculus) | Dorsal | Superior oblique | Depression, intorsion | | CN VI | Pons | Pontomedullary junction | Lateral rectus | Abduction | --- ## Key Clinical Correlations (Brief) * **CN III palsy** → ptosis, dilated pupil, eye down and out * **CN IV palsy** → vertical diplopia, worse on stairs * **CN VI palsy** → inability to abduct eye, medial deviation --- If you want, I can also provide: * **Cavernous sinus relations** * **Brainstem cross-section correlations** * **Clinical case-based MCQs** * **SEO-friendly formatted version for medical websites**
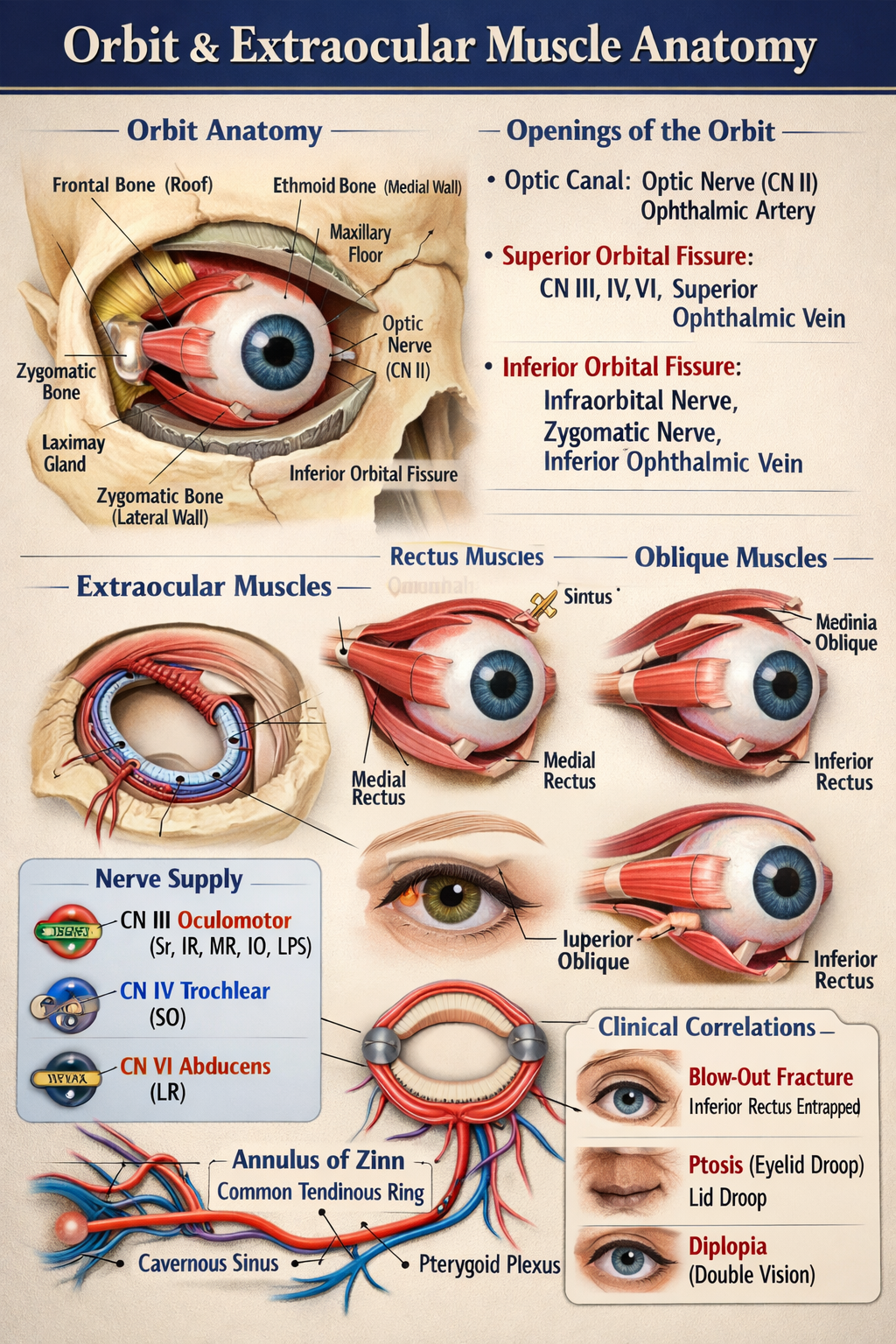
Orbit and Extraocular Muscle Anatomy Explained for Medical Students
## Orbit and Extraocular Muscle Anatomy (Detailed, No Images) --- ## 1. Orbit – Overview The **orbit** is a paired pyramidal bony cavity that houses and protects the eyeball and its associated structures. ### Contents * Eyeball (globe) * Extraocular muscles * Optic nerve (CN II) * Oculomotor (CN III), Trochlear (CN IV), Abducens (CN VI) * Ophthalmic division of trigeminal nerve (CN V1) * Lacrimal gland * Ophthalmic artery and veins * Orbital fat and connective tissue ### Shape and Orientation * **Pyramidal**: base anterior (orbital margin), apex posterior (optic canal) * Apex points medially and posteriorly --- ## 2. Bony Walls of the Orbit ### Roof **Bones:** Frontal bone, lesser wing of sphenoid **Relations:** Anterior cranial fossa, frontal sinus **Structures:** Lacrimal gland fossa, trochlear fossa ### Floor **Bones:** Maxilla, zygomatic, palatine **Relations:** Maxillary sinus **Clinical:** Most common site of blow-out fracture **Structures:** Infraorbital groove and canal ### Medial Wall **Bones:** Ethmoid (lamina papyracea), lacrimal, maxilla, sphenoid **Relations:** Ethmoidal air sinuses **Clinical:** Very thin → spread of infection ### Lateral Wall **Bones:** Zygomatic, greater wing of sphenoid **Strongest wall** **Relations:** Temporal fossa --- ## 3. Openings of the Orbit ### Optic Canal * **Contents:** Optic nerve (CN II), ophthalmic artery * **Location:** Lesser wing of sphenoid ### Superior Orbital Fissure * **Contents:** CN III, IV, V1, VI, superior ophthalmic vein * **Connects:** Middle cranial fossa ### Inferior Orbital Fissure * **Contents:** Infraorbital nerve, zygomatic nerve, inferior ophthalmic vein * **Connects:** Pterygopalatine and infratemporal fossae --- ## 4. Extraocular Muscles – Overview There are **7 extraocular muscles**: * **4 Recti:** Superior, Inferior, Medial, Lateral * **2 Obliques:** Superior, Inferior * **1 Elevator:** Levator palpebrae superioris ### Common Origin * **Annulus of Zinn (Common tendinous ring)** at orbital apex (All recti + levator palpebrae superioris) --- ## 5. Rectus Muscles ### Superior Rectus * **Origin:** Annulus of Zinn * **Insertion:** Superior sclera (anterior to equator) * **Action:** Elevation, adduction, intorsion * **Nerve:** Oculomotor nerve (CN III – superior division) ### Inferior Rectus * **Origin:** Annulus of Zinn * **Insertion:** Inferior sclera * **Action:** Depression, adduction, extorsion * **Nerve:** Oculomotor nerve (CN III – inferior division) ### Medial Rectus * **Origin:** Annulus of Zinn * **Insertion:** Medial sclera * **Action:** Adduction * **Nerve:** Oculomotor nerve (CN III) ### Lateral Rectus * **Origin:** Annulus of Zinn * **Insertion:** Lateral sclera * **Action:** Abduction * **Nerve:** Abducens nerve (CN VI) --- ## 6. Oblique Muscles ### Superior Oblique * **Origin:** Body of sphenoid * **Course:** Passes through trochlea (fibrous pulley) * **Insertion:** Posterosuperolateral sclera * **Action:** Intorsion, depression, abduction * **Nerve:** Trochlear nerve (CN IV) ### Inferior Oblique * **Origin:** Anterior orbital floor (maxilla) * **Insertion:** Posteroinferolateral sclera * **Action:** Extorsion, elevation, abduction * **Nerve:** Oculomotor nerve (CN III) --- ## 7. Levator Palpebrae Superioris * **Origin:** Lesser wing of sphenoid * **Insertion:** Upper eyelid * **Action:** Elevation of upper eyelid * **Nerve:** Oculomotor nerve (CN III – superior division) * **Sympathetic supply:** Müller’s muscle (smooth muscle component) --- ## 8. Blood Supply * **Ophthalmic artery** (branch of internal carotid) * Supplies eyeball, muscles, optic nerve ### Venous Drainage * **Superior and inferior ophthalmic veins** * Drain into cavernous sinus and pterygoid plexus --- ## 9. Nerve Supply Summary (Rule of 3-4-6) * **CN III (Oculomotor):** All extraocular muscles except SO and LR * **CN IV (Trochlear):** Superior oblique * **CN VI (Abducens):** Lateral rectus --- ## 10. Important Clinical Correlations * **Blow-out fracture:** Floor of orbit → inferior rectus entrapment * **Cavernous sinus thrombosis:** Ophthalmic veins involvement * **Ptosis:** CN III palsy or sympathetic damage * **Diplopia:** Extraocular muscle or nerve dysfunction --- If you want, I can next provide **nerve lesions with eye deviation patterns**, **muscle action tables**, **MCQs**, or **SEO-optimized medical content format** for this topic.
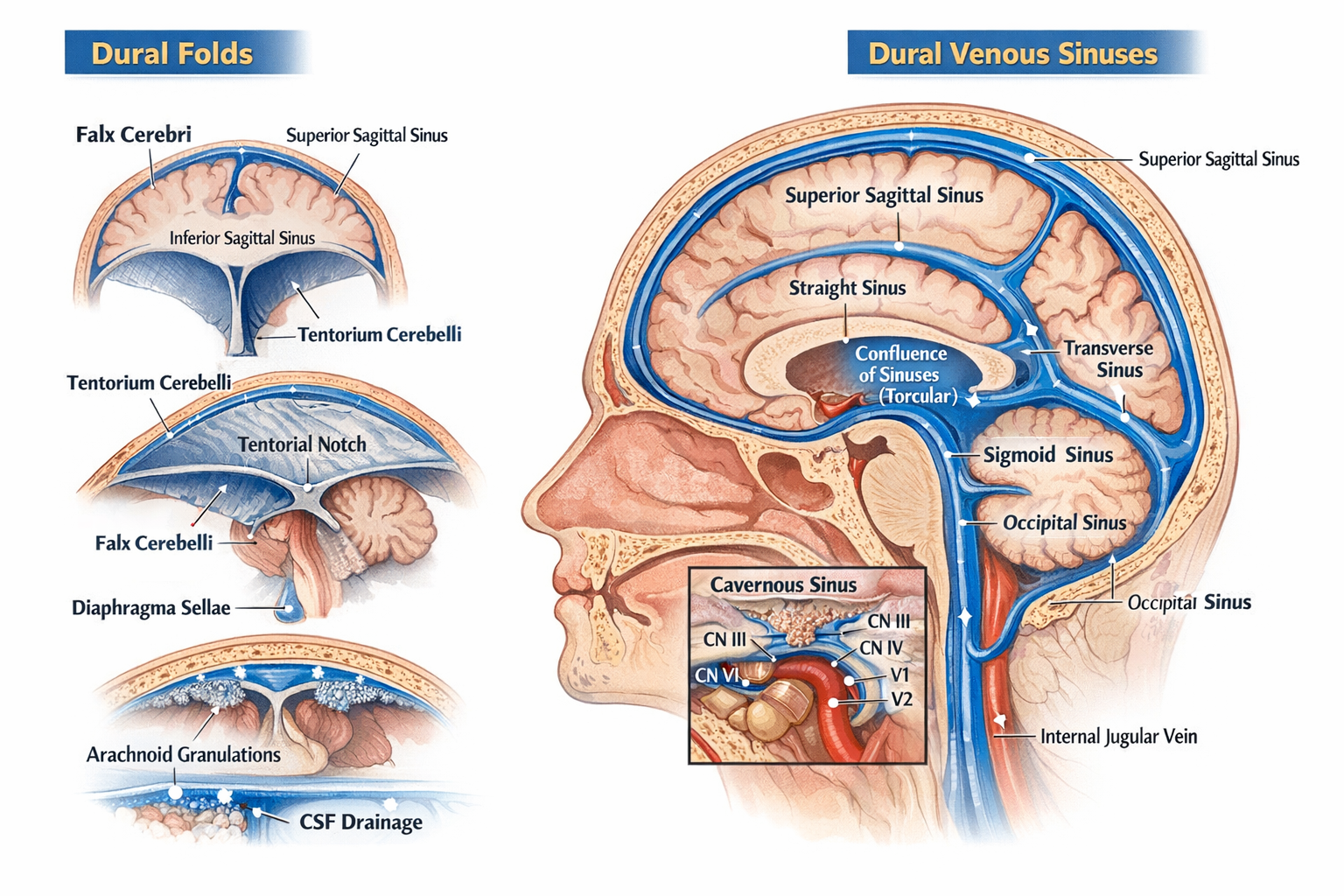
Dural Folds and Dural Venous Sinuses Anatomy, Features and Clinical Significance
## Dural Folds and Dural Venous Sinuses — Complete, Exam-Oriented Anatomy Guide (No Images) --- ## 1. Dura Mater: Brief Context The **dura mater** is the outermost meningeal layer of the brain. It has **two layers**: * **Periosteal (endosteal) layer** – lines the inner surface of the skull * **Meningeal layer** – forms inward folds (**dural folds**) Where these two layers separate, **dural venous sinuses** are formed. 🔗 *Related topic:* [Meninges of Brain](#) --- ## 2. Dural Folds (Dural Septa) Dural folds are **double-layered reflections of meningeal dura mater** that: * Stabilize the brain * Limit excessive movement * Contain venous sinuses at their attachments ### 2.1 Falx Cerebri A **sickle-shaped vertical fold** in the midline. **Attachments** * Anterior: Crista galli of ethmoid * Posterior: Internal occipital protuberance (joins tentorium cerebelli) **Separates** * Right and left cerebral hemispheres **Venous Sinuses Contained** * Superior sagittal sinus (upper border) * Inferior sagittal sinus (free lower border) * Straight sinus (posterior attachment) **Clinical relevance** * Falx meningioma * Subfalcine herniation 🔗 *See also:* [Cerebral Herniation Syndromes](#) --- ### 2.2 Tentorium Cerebelli A **horizontal tent-like fold**. **Attachments** * Anterior: Clinoid processes * Lateral: Superior border of petrous temporal bone * Posterior: Occipital bone **Separates** * Cerebrum (above) from cerebellum (below) **Opening** * Tentorial notch → passage for midbrain **Venous Sinuses Contained** * Transverse sinus * Superior petrosal sinus * Straight sinus (junction with falx cerebri) **Clinical relevance** * Transtentorial (uncal) herniation * Compression of oculomotor nerve 🔗 *Related topic:* [Midbrain Anatomy](#) --- ### 2.3 Falx Cerebelli A **small vertical fold** below the tentorium. **Attachments** * Internal occipital crest **Separates** * Two cerebellar hemispheres (partially) **Venous Sinus** * Occipital sinus --- ### 2.4 Diaphragma Sellae A **small circular dural fold** forming the roof of sella turcica. **Central opening** * Allows passage of pituitary stalk (infundibulum) **Clinical relevance** * Pituitary adenoma expansion * CSF leak after trans-sphenoidal surgery 🔗 *See also:* [Pituitary Gland Anatomy](#) --- ## 3. Dural Venous Sinuses ### Definition **Endothelial-lined venous channels** between layers of dura mater that drain venous blood from brain, meninges, and skull. **Key characteristics** * No valves * No muscular layer * Rigid walls (do not collapse) --- ## 4. Classification of Dural Venous Sinuses ### 4.1 Unpaired Sinuses #### Superior Sagittal Sinus * Location: Upper margin of falx cerebri * Drains: Cerebral veins, CSF via arachnoid granulations * Ends in: Confluence of sinuses **Clinical** * Site of CSF absorption * Thrombosis → raised intracranial pressure --- #### Inferior Sagittal Sinus * Location: Free lower margin of falx cerebri * Drains into: Straight sinus --- #### Straight Sinus * Formed by union of inferior sagittal sinus + great cerebral vein (of Galen) * Ends in: Confluence of sinuses --- #### Occipital Sinus * Smallest sinus * Located in falx cerebelli --- ### 4.2 Paired Sinuses #### Transverse Sinuses * Located along posterolateral margin of tentorium * Drain into: Sigmoid sinuses --- #### Sigmoid Sinuses * S-shaped * Continue as: Internal jugular veins 🔗 *Related topic:* [Internal Jugular Vein](#) --- #### Cavernous Sinus (Highly Important) Located on either side of body of sphenoid. **Contents** * Internal carotid artery * CN VI (abducent nerve) **Lateral wall (superior to inferior)** * CN III * CN IV * V1 * V2 **Drains** * Superior & inferior ophthalmic veins **Clinical** * Cavernous sinus thrombosis * Carotid–cavernous fistula 🔗 *See also:* [Cranial Nerves in Cavernous Sinus](#) --- #### Petrosal Sinuses * **Superior petrosal sinus**: cavernous → transverse * **Inferior petrosal sinus**: cavernous → internal jugular vein --- ## 5. Confluence of Sinuses (Torcular Herophili) * Located at internal occipital protuberance * Receives: * Superior sagittal sinus * Straight sinus * Occipital sinus * Drains into: Transverse sinuses --- ## 6. CSF Drainage and Arachnoid Granulations * CSF absorbed into **superior sagittal sinus** * Via arachnoid villi and granulations 🔗 *Related topic:* [CSF Circulation and Absorption](#) --- ## 7. Clinical Correlation Summary | Condition | Related Structure | | ----------------- | -------------------------- | | Raised ICP | Superior sagittal sinus | | Uncal herniation | Tentorium cerebelli | | Diplopia | Cavernous sinus (CN VI) | | CSF leak | Diaphragma sellae | | Venous thrombosis | Sagittal / cavernous sinus | --- ## 8. One-Line Exam Pearls * Dural folds are formed by **meningeal dura only** * Venous sinuses lack valves and smooth muscle * Cavernous sinus is the **only sinus containing cranial nerves** * Falx cerebri contains **two sagittal sinuses** --- If you want, I can next provide: * **SEO title, meta description, and long-tail keywords** * **20 hard MCQs (including case-based)** * **FAQ schema JSON** * **Internal link structure optimized for a medical website**
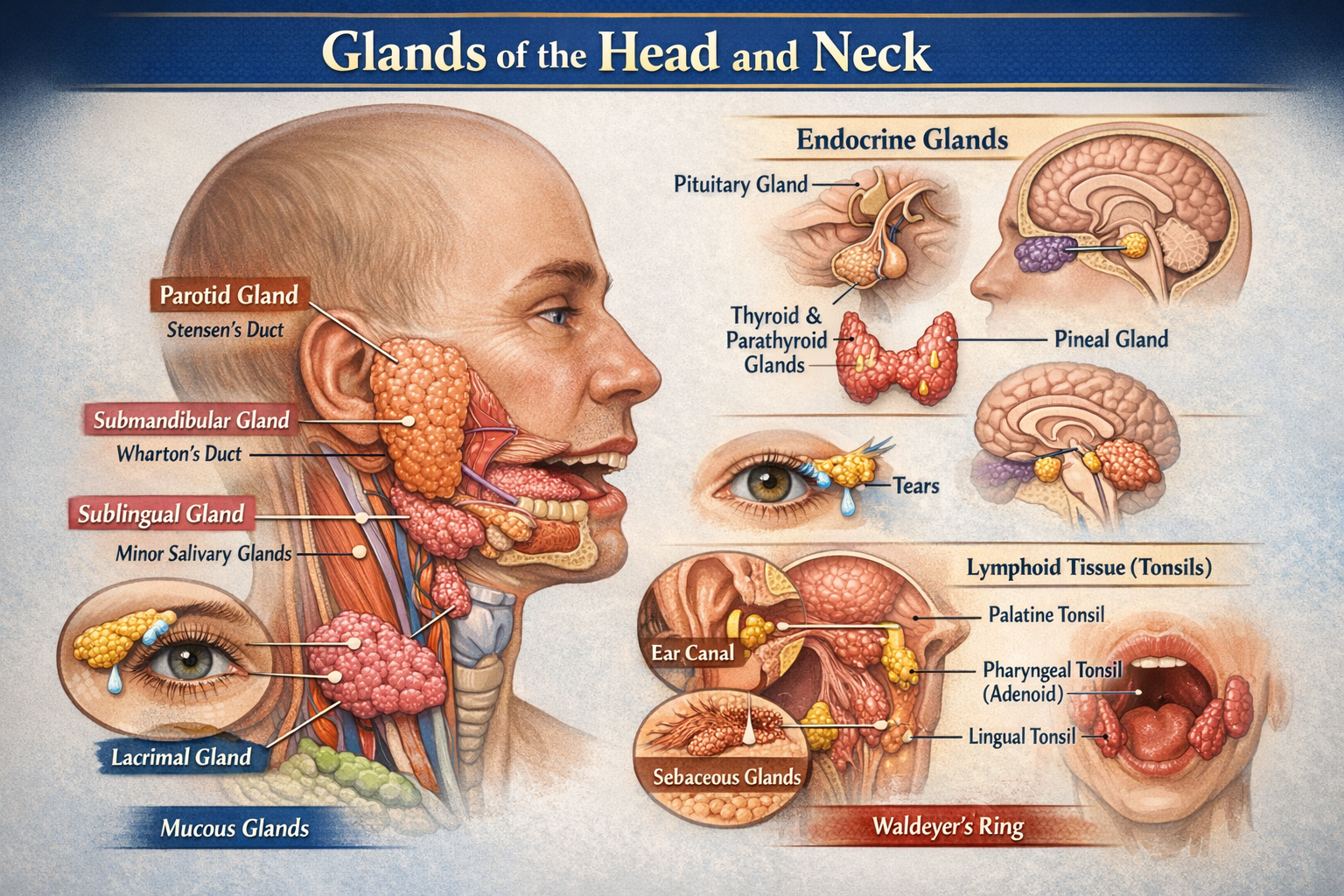
Glands of Head and Neck Anatomy Types Functions and Clinical Importance
Below is a **clear, exam-oriented yet complete description of the glands in the head and neck**, **without images**, suitable for **medical students, anatomy revision, and clinical correlation**. --- # Glands of the Head and Neck – Detailed Anatomy Glands in the head and neck are primarily **exocrine glands** involved in **saliva production, lubrication, immunity, thermoregulation, and endocrine regulation**. They are classified into **salivary glands, endocrine glands, mucous glands, sebaceous glands, and specialized glands**. --- ## I. SALIVARY GLANDS Responsible for saliva secretion → lubrication, digestion (amylase), oral hygiene. ### A. Major Salivary Glands #### 1. Parotid Gland * **Largest salivary gland** * **Type:** Pure serous * **Location:** * In the **parotid bed** * Anterior to ear, posterior to ramus of mandible * **Relations (Superficial to deep):** * Skin → fascia → facial nerve → retromandibular vein → external carotid artery * **Duct:** Stensen’s duct * Opens opposite **upper second molar** * **Nerve supply:** * Parasympathetic: Glossopharyngeal nerve (CN IX) via **otic ganglion** * **Clinical relevance:** * Parotitis (mumps) * Facial nerve injury during surgery --- #### 2. Submandibular Gland * **Type:** Mixed (predominantly serous) * **Location:** * Submandibular triangle * Superficial and deep parts around **mylohyoid muscle** * **Duct:** Wharton’s duct * Opens at **sublingual papilla** * **Nerve supply:** * Parasympathetic: Facial nerve (CN VII) via **chorda tympani** * **Clinical relevance:** * Common site of **salivary stones (sialolithiasis)** --- #### 3. Sublingual Gland * **Smallest major gland** * **Type:** Mixed (predominantly mucous) * **Location:** * Floor of mouth * Beneath mucosa, above mylohyoid * **Ducts:** Multiple ducts of Rivinus * **Nerve supply:** * Facial nerve (CN VII) * **Clinical relevance:** * Ranula (mucous cyst) --- ### B. Minor Salivary Glands * Numerous small glands embedded in mucosa * **Locations:** * Lips * Cheeks * Tongue * Soft palate * **Type:** Mostly mucous * **Clinical importance:** * Tumors (often malignant) --- ## II. ENDOCRINE GLANDS OF HEAD AND NECK ### 1. Thyroid Gland * **Largest endocrine gland** * **Location:** * Anterior neck * Opposite C5–T1 vertebrae * **Structure:** * Two lobes + isthmus * **Hormones:** * T3, T4 → metabolism * Calcitonin → calcium regulation * **Blood supply:** * Superior thyroid artery * Inferior thyroid artery * **Clinical relevance:** * Goiter * Hypothyroidism, hyperthyroidism --- ### 2. Parathyroid Glands * Usually **four glands** * **Location:** * Posterior surface of thyroid * **Hormone:** * Parathyroid hormone (PTH) * **Function:** * Increases blood calcium * **Clinical relevance:** * Hypocalcemia after thyroid surgery --- ### 3. Pituitary Gland * **Master endocrine gland** * **Location:** * Sella turcica of sphenoid bone * **Divisions:** * Anterior pituitary * Posterior pituitary * **Function:** * Controls growth, reproduction, stress response * **Clinical relevance:** * Pituitary adenomas --- ### 4. Pineal Gland * **Location:** * Roof of third ventricle * **Hormone:** * Melatonin * **Function:** * Circadian rhythm regulation --- ## III. MUCOUS GLANDS ### Nasal Glands * Found in nasal mucosa * Produce mucus to humidify air ### Palatine Glands * Located in soft palate * Lubricate food during swallowing --- ## IV. SEBACEOUS GLANDS * Associated with hair follicles * Abundant on: * Face * Scalp * Produce **sebum** * **Clinical relevance:** * Acne vulgaris * Sebaceous cysts --- ## V. SWEAT GLANDS (MODIFIED) ### Ceruminous Glands * Located in **external auditory canal** * Produce **ear wax (cerumen)** * Protect tympanic membrane --- ## VI. SPECIALIZED GLANDS ### Lacrimal Gland * Produces tears * Located in **superolateral orbit** * Drains into conjunctival sac * **Clinical relevance:** Dry eye syndrome --- ## VII. LYMPHOID GLANDULAR STRUCTURES ### Tonsils (Waldeyer’s Ring) * Palatine tonsils * Pharyngeal tonsil (adenoids) * Lingual tonsils * Function: Immune defense --- ## SUMMARY TABLE | Gland | Type | Function | | ------------- | --------- | ---------------- | | Parotid | Serous | Saliva (amylase) | | Submandibular | Mixed | Saliva | | Sublingual | Mucous | Lubrication | | Thyroid | Endocrine | Metabolism | | Parathyroid | Endocrine | Calcium balance | | Pituitary | Endocrine | Hormonal control | | Lacrimal | Exocrine | Tear secretion | --- If you want next: * **SEO-friendly version** * **MCQs (case-based)** * **FAQ JSON schema** * **Embryological development** * **Clinical correlations only** Just tell me 👍
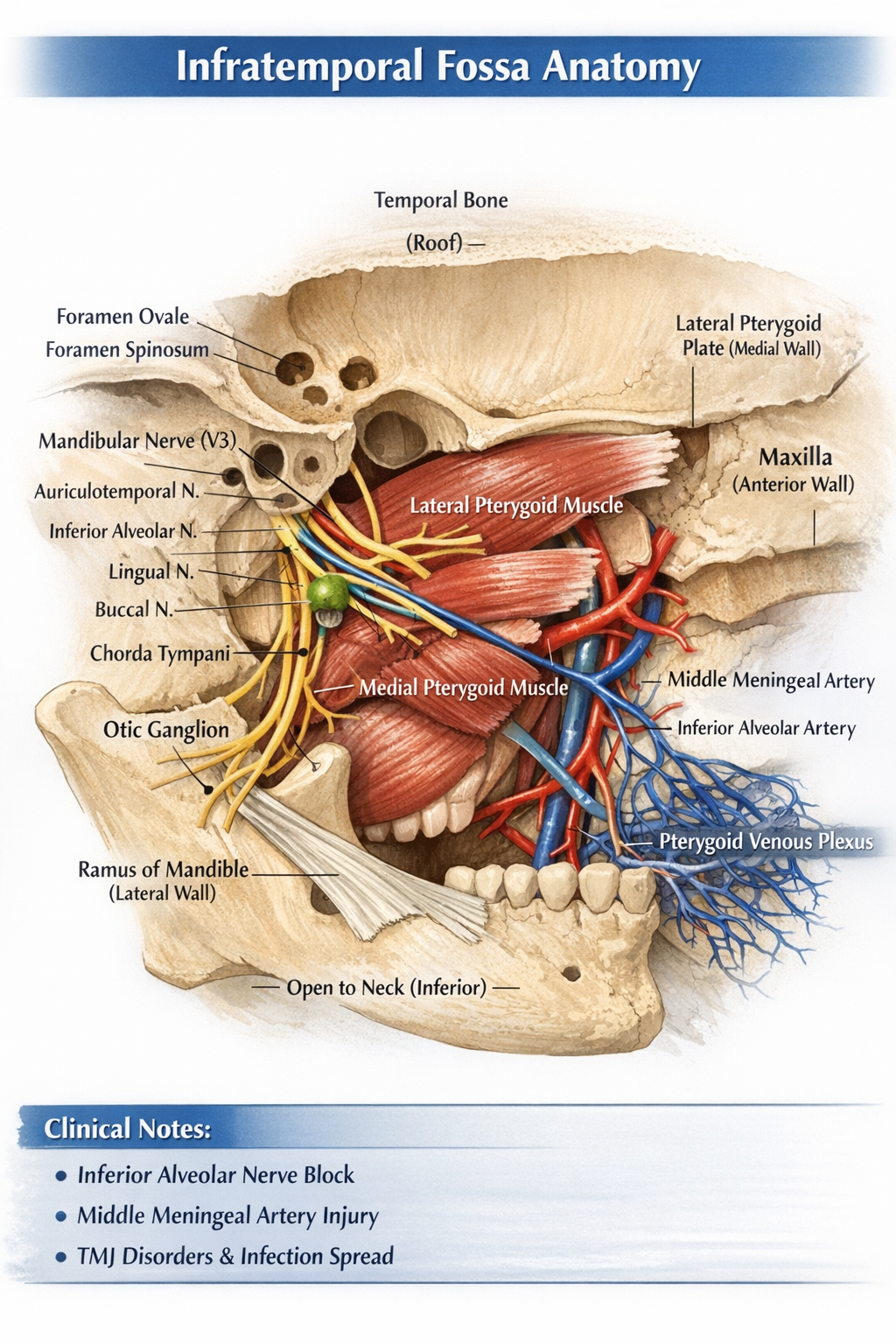
Infratemporal Fossa Anatomy Boundaries Contents Nerves Vessels and Clinical Importance
## Infratemporal Fossa – Detailed Anatomy (No Images) ### **Definition** The **infratemporal fossa** is an irregular, wedge-shaped deep space located **below the base of the skull**, **medial to the ramus of the mandible**, and **posterior to the maxilla**. It is a major neurovascular and muscular compartment involved in **mastication, facial sensation, and cranial–facial circulation**. --- ## **Boundaries** ### **Roof (Superior)** * **Infratemporal surface of greater wing of sphenoid** * **Squamous part of temporal bone** * Contains: * **Foramen ovale** – mandibular nerve (V3), accessory meningeal artery, lesser petrosal nerve * **Foramen spinosum** – middle meningeal artery and vein, meningeal branch of V3 ### **Lateral Wall** * **Ramus of mandible** ### **Medial Wall** * **Lateral pterygoid plate (sphenoid)** * **Tensor veli palatini muscle** ### **Anterior Wall** * **Posterior surface of maxilla** ### **Posterior Wall** * **Tympanic plate** * **Mastoid and styloid processes of temporal bone** * Separates infratemporal fossa from **parotid region** ### **Inferior Boundary** * **Open** (continuous with tissues of the neck) --- ## **Contents** ### **Muscles of Mastication** 1. **Medial pterygoid** * Origin: medial surface of lateral pterygoid plate * Insertion: medial surface of mandibular angle * Action: elevation and protrusion of mandible 2. **Lateral pterygoid** * Two heads: * Superior: greater wing of sphenoid * Inferior: lateral pterygoid plate * Insertion: neck of mandible and TMJ disc * Action: depression, protrusion, lateral movement of mandible 3. **Lower part of temporalis** (tendon passing through fossa) --- ## **Nerves** ### **Mandibular Nerve (V3) – Main Nerve** Exits skull via **foramen ovale** #### **Branches** * **Auriculotemporal nerve** – sensation to temporal region and TMJ * **Inferior alveolar nerve** * Gives **nerve to mylohyoid** * Enters mandibular foramen * **Lingual nerve** – general sensation to anterior 2/3 of tongue * **Buccal nerve** – sensory to cheek * **Motor branches** to muscles of mastication ### **Chorda Tympani (Facial nerve branch)** * Joins lingual nerve * Carries: * Taste fibers (anterior 2/3 of tongue) * Parasympathetic fibers to submandibular and sublingual glands ### **Otic Ganglion** * Parasympathetic ganglion * Related to mandibular nerve * Secretomotor supply to **parotid gland** via auriculotemporal nerve --- ## **Arteries** ### **Maxillary Artery (Terminal branch of external carotid)** Major arterial content of infratemporal fossa #### **Branches (Mandibular Part)** * **Deep auricular artery** * **Anterior tympanic artery** * **Middle meningeal artery** * **Accessory meningeal artery** * **Inferior alveolar artery** --- ## **Veins** ### **Pterygoid Venous Plexus** * Extensive venous network * Drains into **maxillary vein** * Communicates with: * Cavernous sinus (via emissary veins) * Clinical relevance: spread of infection --- ## **Ligaments** * **Sphenomandibular ligament** * Extends from spine of sphenoid to lingula of mandible * Separates inferior alveolar nerve from lingual nerve --- ## **Communications** | Communication | Opening | Connects With | | --------------------- | ------------------------ | ------------------------------ | | Middle cranial fossa | Foramen ovale | V3, lesser petrosal nerve | | Middle cranial fossa | Foramen spinosum | Middle meningeal artery | | Pterygopalatine fossa | Pterygomaxillary fissure | Maxillary nerve and vessels | | Orbit | Inferior orbital fissure | Infraorbital nerve and vessels | | Temporal fossa | Deep to zygomatic arch | Temporalis muscle | --- ## **Clinical Importance** * **Inferior alveolar nerve block** administered in infratemporal fossa * **Middle meningeal artery injury** → extradural hematoma * **TMJ disorders** involve lateral pterygoid * **Spread of infection** via pterygoid venous plexus to cavernous sinus * **Trigeminal neuralgia** may involve V3 branches --- ## **Summary** The infratemporal fossa is a complex anatomical space housing **muscles of mastication, the mandibular nerve and its branches, maxillary artery, pterygoid venous plexus, and parasympathetic ganglia**. It plays a crucial role in **chewing, facial sensation, salivation, and cranial circulation**, and is of high **clinical and surgical significance**. If you want, I can also provide **SEO title, MCQs (case-based), FAQ JSON, or exam-oriented tables** for this topic.
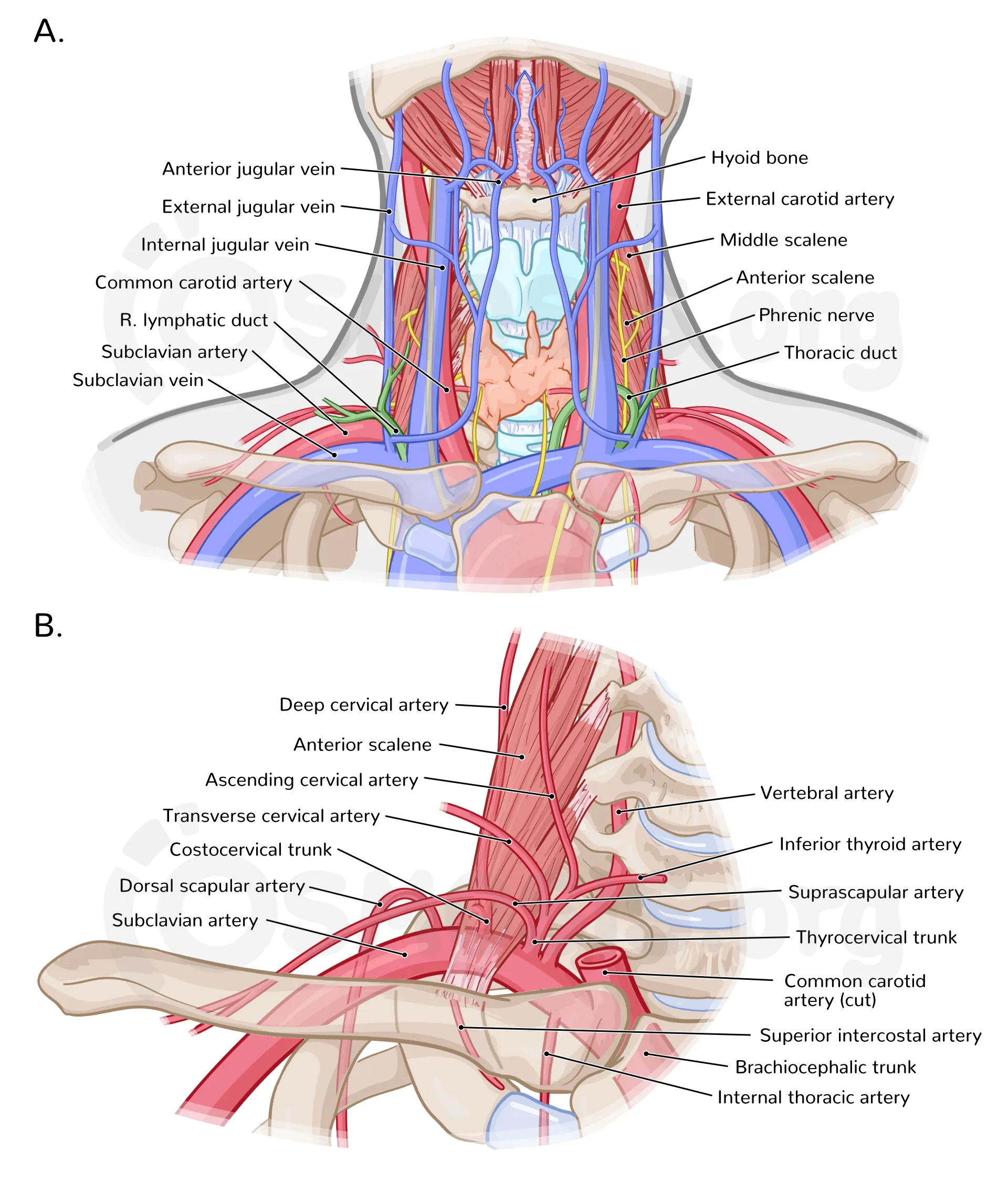
Neurovascular Structures of the Neck Anatomy Clinical Importance and Exam Guide
Below is a **concise but complete, exam-oriented explanation** of **neurovascular structures of the neck**, written **without images**, covering **arteries, veins, nerves, and key clinical correlations** in one place. --- ## Neurovascular Structures of the Neck The neck contains vital **arterial, venous, and neural structures** that connect the brain with the rest of the body. These structures are arranged in **distinct fascial compartments**, most importantly within the **carotid sheath**. --- ## 1. Arterial Structures of the Neck ### A. Common Carotid Arteries (CCA) * **Origin** * Right: From **brachiocephalic trunk** * Left: From **arch of aorta** * **Course** * Ascend in the neck within the **carotid sheath** * Divide at **C4 vertebral level** (upper border of thyroid cartilage) * **Termination** * External carotid artery * Internal carotid artery --- ### B. External Carotid Artery (ECA) * Supplies **structures of face, scalp, neck** * Lies **anteromedial** to internal carotid initially **Branches (Mnemonic: *Some Angry Lady Figured Out PMS*)** 1. Superior thyroid 2. Ascending pharyngeal 3. Lingual 4. Facial 5. Occipital 6. Posterior auricular 7. Maxillary 8. Superficial temporal --- ### C. Internal Carotid Artery (ICA) * Supplies **brain and eye** * **No branches in the neck** * Enters skull via **carotid canal** * Clinical importance: **stroke, carotid stenosis** --- ### D. Subclavian Artery (Neck Part) **Major branches** * Vertebral artery → brainstem, posterior brain * Thyrocervical trunk * Costocervical trunk --- ## 2. Venous Structures of the Neck ### A. Internal Jugular Vein (IJV) * Drains **brain, face, neck** * Lies **lateral to common carotid artery** * Joins subclavian vein → **brachiocephalic vein** * Important landmark for **central venous access** --- ### B. External Jugular Vein (EJV) * Drains scalp and face * Superficial, crosses sternocleidomastoid * Visible in raised venous pressure --- ### C. Anterior Jugular Veins * Drain submental region * May form **jugular venous arch** --- ## 3. Neural Structures of the Neck ### A. Cranial Nerves in the Neck #### 1. Vagus Nerve (CN X) * Lies **between carotid artery and jugular vein** * Supplies: * Parasympathetic to thoracic and abdominal organs * Laryngeal branches (voice) #### 2. Glossopharyngeal Nerve (CN IX) * Supplies: * Stylopharyngeus * Taste posterior 1/3 tongue * Carotid body & sinus #### 3. Accessory Nerve (CN XI) * Supplies: * Sternocleidomastoid * Trapezius * Vulnerable during **neck surgeries** #### 4. Hypoglossal Nerve (CN XII) * Motor to tongue muscles * Injury causes **tongue deviation** --- ### B. Cervical Plexus (C1–C4) * Located deep to sternocleidomastoid * **Sensory branches** * Lesser occipital * Great auricular * Transverse cervical * Supraclavicular * **Motor branches** * Ansa cervicalis → infrahyoid muscles * Phrenic nerve (C3–C5) → diaphragm --- ### C. Brachial Plexus (Neck Part) * Roots: **C5–T1** * Lies between **anterior and middle scalene muscles** * Supplies **upper limb** --- ### D. Sympathetic Trunk * Lies posterior to carotid sheath * Cervical ganglia: * Superior * Middle * Inferior (stellate) * Injury → **Horner syndrome** * Ptosis * Miosis * Anhidrosis --- ## 4. Carotid Sheath – Core Neurovascular Bundle ### Contents * Common/Internal carotid artery (medial) * Internal jugular vein (lateral) * Vagus nerve (posterior) * Deep cervical lymph nodes * Carotid plexus (sympathetic fibers) ### Clinical relevance * Carotid endarterectomy * Central line placement * Neck trauma --- ## 5. Important Clinical Correlations * **Carotid sinus**: Baroreceptor → BP regulation * **Carotid body**: Chemoreceptor → oxygen sensing * **Neck hematoma**: Can compress airway * **Surgical risk**: Accessory nerve injury → shoulder droop --- ## Quick Summary Table | Structure | Function | | ----------------- | ------------------------- | | Carotid arteries | Brain & face blood supply | | Jugular veins | Venous drainage of head | | Vagus nerve | Parasympathetic, voice | | Cervical plexus | Neck sensation & movement | | Sympathetic trunk | Autonomic control | --- If you want next: * **Exam-oriented MCQs** * **Clinical case-based questions** * **SEO-optimized version** * **FAQ JSON** * **HTML/CSS/JS interactive content** Just tell me.
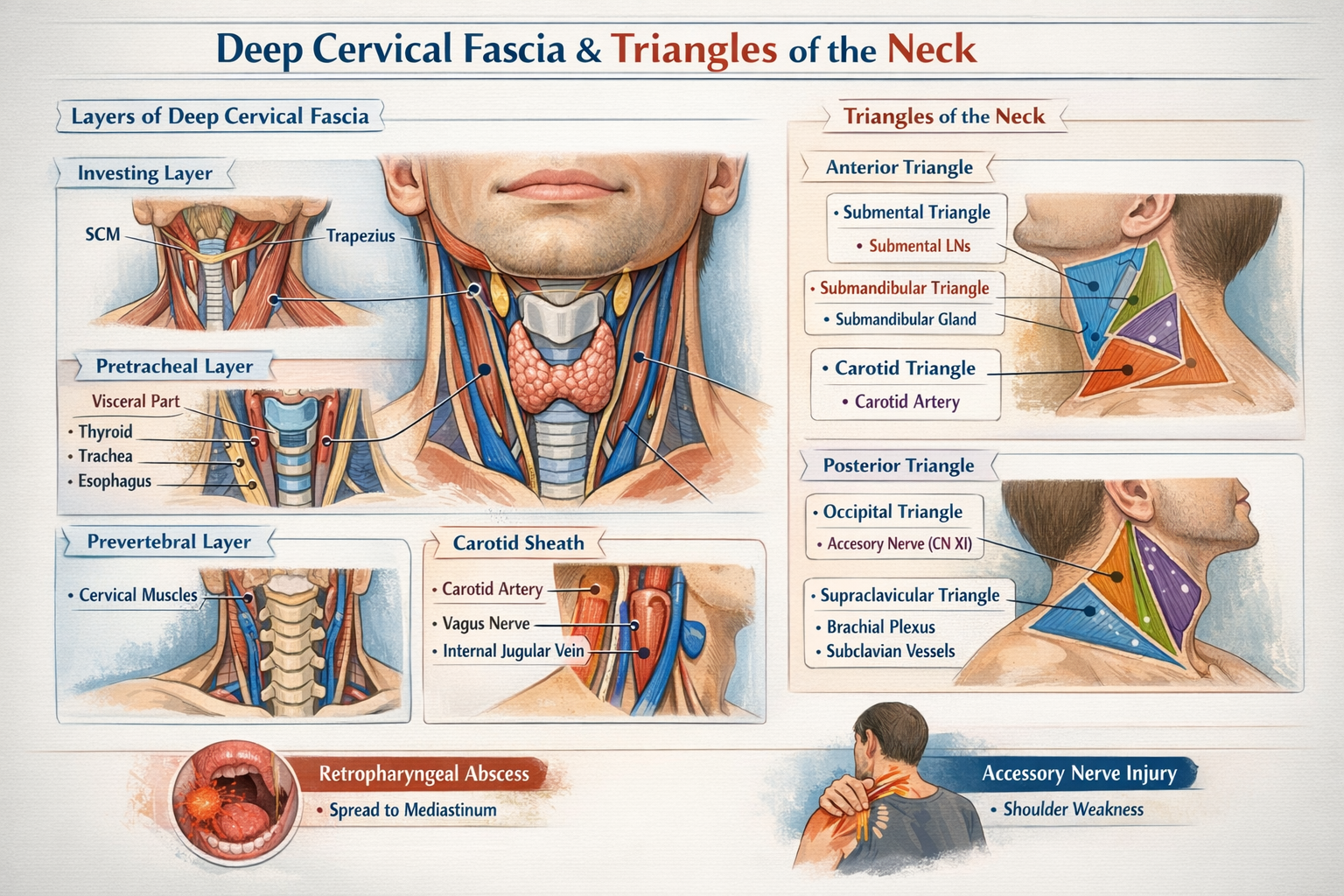
Deep Cervical Fascia and Triangles of the Neck Anatomy Explained in Detail
## Deep Cervical Fascia and Triangles of the Neck — Detailed Anatomical Guide --- # **Deep Cervical Fascia** ### **Definition** The **deep cervical fascia** is a dense connective tissue layer in the neck that surrounds, supports, and compartmentalizes muscles, vessels, nerves, and viscera. It plays a critical role in structural support, movement coordination, and containment of infections. --- ## **Layers of Deep Cervical Fascia** ### **1. Investing Layer (Superficial Layer of Deep Fascia)** **Extent** * Encloses the entire neck like a collar * Splits to surround **sternocleidomastoid (SCM)** and **trapezius** * Extends: * Superiorly: superior nuchal line, mandible, zygomatic arch * Inferiorly: clavicle, sternum, acromion **Attachments** * Mastoid process * External occipital protuberance * Lower border of mandible * Spine of scapula **Structures Enclosed** * SCM * Trapezius * Parotid gland (forms parotid fascia) * Submandibular gland (forms submandibular fascia) **Clinical Importance** * Limits superficial spread of infection * Parotid abscess causes severe pain due to tight fascia * Forms stylomandibular ligament --- ### **2. Pretracheal Layer** Divided into **muscular** and **visceral** parts. #### **A. Muscular Part** **Encloses** * Infrahyoid (strap) muscles: * Sternohyoid * Sternothyroid * Thyrohyoid * Omohyoid **Extent** * Hyoid bone → superior mediastinum --- #### **B. Visceral Part** **Encloses** * Thyroid gland * Trachea * Esophagus **Special Features** * Forms **false capsule of thyroid** * Thickened posteriorly to form **Berry’s ligament** (anchors thyroid to cricoid cartilage) **Clinical Importance** * Explains movement of thyroid gland during swallowing * Thyroid swelling moves with deglutition --- ### **3. Prevertebral Layer** **Extent** * Base of skull → T3 vertebra **Encloses** * Cervical vertebrae * Deep neck muscles: * Longus colli * Longus capitis * Scalene muscles * Vertebral vessels * Cervical sympathetic trunk **Lateral Extension** * Forms **axillary sheath**, enclosing: * Subclavian artery * Brachial plexus **Clinical Importance** * Infection here can spread to posterior mediastinum * Involvement affects neck movements --- ### **4. Carotid Sheath** A tubular condensation of deep cervical fascia formed by: * Investing layer * Pretracheal layer * Prevertebral layer **Extent** * Base of skull → root of neck **Contents** * Common carotid artery (internal carotid above bifurcation) * Internal jugular vein * Vagus nerve * Deep cervical lymph nodes * Sympathetic fibers **Arrangement** * Artery: medial * Vein: lateral * Nerve: posterior **Clinical Importance** * Compression can affect cerebral blood flow * Infections can spread vertically --- ## **Spaces Formed by Deep Cervical Fascia** * **Pretracheal space** → anterior mediastinum * **Retropharyngeal space** → posterior mediastinum (danger space) * **Prevertebral space** → posterior mediastinum --- # **Triangles of the Neck** The neck is divided by **sternocleidomastoid (SCM)** into **anterior** and **posterior triangles**. --- ## **Anterior Triangle** ### **Boundaries** * Medial: midline of neck * Lateral: anterior border of SCM * Superior: lower border of mandible * Apex: suprasternal notch ### **Roof** * Skin * Superficial fascia * Platysma * Investing layer of deep fascia ### **Floor** * Pharynx * Larynx * Thyroid gland --- ### **Subdivisions of Anterior Triangle** --- ### **1. Submental Triangle** **Boundaries** * Two anterior bellies of digastric * Base: body of hyoid **Contents** * Submental lymph nodes * Small veins forming anterior jugular vein **Clinical Importance** * Drains lower lip, chin, tip of tongue --- ### **2. Submandibular (Digastric) Triangle** **Boundaries** * Anterior and posterior bellies of digastric * Lower border of mandible **Contents** * Submandibular gland * Facial artery and vein * Hypoglossal nerve * Submandibular lymph nodes --- ### **3. Carotid Triangle** **Boundaries** * Posterior belly of digastric * Superior belly of omohyoid * Anterior border of SCM **Contents** * Common carotid artery and bifurcation * Internal and external carotid arteries * Internal jugular vein * Vagus nerve * Hypoglossal nerve * Carotid sinus and body **Clinical Importance** * Site for carotid pulse * Carotid endarterectomy --- ### **4. Muscular Triangle** **Boundaries** * Midline of neck * Anterior border of SCM * Superior belly of omohyoid **Contents** * Infrahyoid muscles * Thyroid and parathyroid glands * Larynx * Trachea --- ## **Posterior Triangle** ### **Boundaries** * Anterior: posterior border of SCM * Posterior: anterior border of trapezius * Inferior: clavicle * Apex: where SCM and trapezius meet ### **Roof** * Skin * Superficial fascia * Platysma * Investing layer of deep fascia ### **Floor** * Splenius capitis * Levator scapulae * Scalene muscles --- ### **Subdivision of Posterior Triangle** --- ### **1. Occipital Triangle** **Boundaries** * SCM * Trapezius * Inferior belly of omohyoid **Contents** * Spinal accessory nerve (CN XI) * Cervical plexus branches * Occipital artery * Lymph nodes **Clinical Importance** * CN XI injury causes shoulder droop --- ### **2. Supraclavicular (Subclavian) Triangle** **Boundaries** * Clavicle * SCM * Inferior belly of omohyoid **Contents** * Subclavian artery and vein * Brachial plexus trunks * Supraclavicular lymph nodes **Clinical Importance** * Venous access * Pancoast tumor involvement --- ## **Key Clinical Correlations (High-Yield)** * Deep cervical fascia directs spread of neck infections * Retropharyngeal abscess can descend into mediastinum * Thyroid movement with swallowing explained by pretracheal fascia * Accessory nerve vulnerability in posterior triangle * Carotid sheath protects vital neurovascular structures --- If you want, I can also provide: * **SEO-optimized title, description, keywords** * **Hard MCQs with case-based questions (HTML/CSS/JS)** * **FAQ in JSON schema format** * **One-page exam revision notes** Just tell me 👍
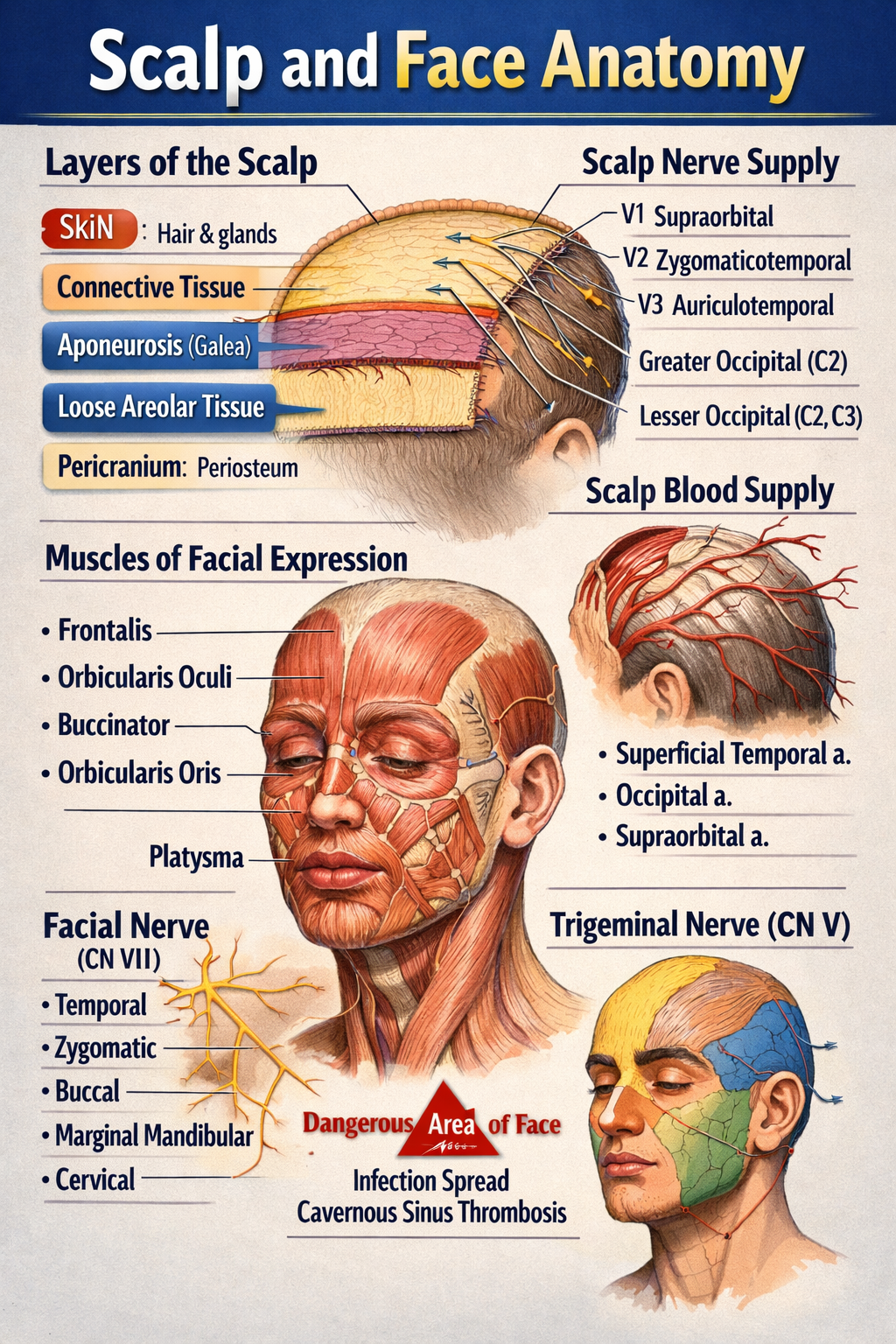
Scalp and Face Anatomy Complete Structure Nerves Blood Supply and Clinical Correlation
Below is a **complete, structured, exam-oriented yet clinically relevant explanation of SCALP AND FACE ANATOMY** — **text only, no images**, written clearly for medical students and healthcare learners. --- # SCALP AND FACE ANATOMY – COMPLETE DETAILED GUIDE --- ## PART A: SCALP ANATOMY ### 1. Definition The **scalp** is the soft tissue covering the cranial vault, extending: * **Anteriorly**: up to the supraorbital margins * **Posteriorly**: to the superior nuchal lines * **Laterally**: to the zygomatic arches --- ### 2. Layers of the Scalp (Mnemonic: **SCALP**) 1. **S – Skin** * Thick, hair-bearing * Rich in sebaceous and sweat glands * Contains hair follicles * Highly vascular → profuse bleeding from cuts 2. **C – Connective Tissue (Dense)** * Fibrofatty layer * Contains **blood vessels and nerves** * Vessels are fixed → cannot retract → excessive bleeding 3. **A – Aponeurosis (Galea Aponeurotica)** * Tough fibrous sheet * Connects: * **Frontalis muscle (anterior)** * **Occipitalis muscle (posterior)** * Lacerations here gape widely 4. **L – Loose Areolar Tissue** * Also called **“danger area of scalp”** * Allows movement of upper 3 layers * Contains emissary veins → connects scalp veins to intracranial venous sinuses * Infection may spread → **cavernous sinus thrombosis / meningitis** 5. **P – Pericranium** * Periosteum covering skull bones * Loosely attached except at sutures * Subperiosteal hematoma limited by sutures --- ### 3. Muscles of the Scalp **Occipitofrontalis muscle** * Frontal belly: elevates eyebrows, wrinkles forehead * Occipital belly: retracts scalp * Innervation: **Facial nerve (CN VII)** --- ### 4. Blood Supply of Scalp #### Arteries (ECA + ICA branches) * **From External Carotid Artery** * Superficial temporal artery * Posterior auricular artery * Occipital artery * **From Internal Carotid Artery (Ophthalmic branch)** * Supraorbital artery * Supratrochlear artery --- ### 5. Venous Drainage * Superficial temporal vein * Posterior auricular vein * Occipital vein → drain into **external jugular vein** **Emissary veins** * Connect extracranial veins to intracranial sinuses * Pathway for infection spread --- ### 6. Nerve Supply of Scalp #### Sensory (Trigeminal + Cervical nerves) * **Anterior to auricle** * Supraorbital nerve (V1) * Supratrochlear nerve (V1) * Zygomaticotemporal nerve (V2) * Auriculotemporal nerve (V3) * **Posterior to auricle** * Greater occipital nerve (C2) * Lesser occipital nerve (C2) * Third occipital nerve (C3) #### Motor * Facial nerve (CN VII) → occipitofrontalis --- ### 7. Applied Anatomy of Scalp * Scalp wounds bleed profusely * Loose areolar tissue → danger area * Cephalhematoma (subperiosteal) * Caput succedaneum (superficial swelling) --- --- ## PART B: FACE ANATOMY --- ### 1. Definition The **face** is the anterior part of the head extending: * From the hairline to the chin * Between the ears laterally --- ### 2. Muscles of Facial Expression * Derived from **second pharyngeal arch** * Insert into skin → facial expressions * Supplied by **Facial nerve (CN VII)** #### Major Groups **Orbital group** * Orbicularis oculi (closes eye) **Oral group** * Orbicularis oris (closes mouth) * Buccinator (cheek muscle) **Nasal group** * Nasalis * Levator labii superioris alaeque nasi --- ### 3. Blood Supply of Face #### Arteries (External Carotid mainly) * Facial artery * Superficial temporal artery * Maxillary artery **Dangerous area of face** * Upper lip, nose, medial cheek * Infection may spread via angular vein → cavernous sinus --- ### 4. Venous Drainage of Face * Facial vein * Angular vein * Retromandibular vein **Communicates with cavernous sinus via** * Ophthalmic veins --- ### 5. Nerve Supply of Face #### Sensory – Trigeminal Nerve (CN V) * **Ophthalmic (V1)**: forehead, upper eyelid * **Maxillary (V2)**: cheek, upper lip * **Mandibular (V3)**: lower lip, chin #### Motor – Facial Nerve (CN VII) Branches within parotid gland: * Temporal * Zygomatic * Buccal * Marginal mandibular * Cervical (Mnemonic: **To Zanzibar By Motor Car**) --- ### 6. Lymphatic Drainage of Face * Submental nodes (chin, lower lip) * Submandibular nodes (cheeks, upper lip) * Preauricular nodes (lateral face) --- ### 7. Skin of Face * Thin, highly vascular * Rich sebaceous glands * Heals well with minimal scarring --- ### 8. Applied Anatomy of Face * Bell’s palsy → facial nerve paralysis * Trigeminal neuralgia * Cavernous sinus thrombosis * Facial nerve injury during parotid surgery * Acne common due to sebaceous glands --- ## QUICK EXAM SUMMARY * **Scalp layers**: Skin, Connective tissue, Aponeurosis, Loose areolar tissue, Pericranium * **Danger areas**: Loose areolar tissue of scalp, Central face * **Motor nerve of face**: Facial nerve (CN VII) * **Sensory nerve of face**: Trigeminal nerve (CN V) * **Main artery of face**: Facial artery --- If you want next: * **MCQs (hard + case based)** * **Clinical correlations only** * **Embryological basis** * **SEO-optimized version** * **Notes in table format** Just tell me 👍
Browse by Medical Category
Explore content organized by medical specialties and systems